Preclinical models of pancreatic ductal adenocarcinoma
Introduction
Pancreatic ductal adenocarcinoma (PDAC) accounts for upwards of 90% of all pancreatic malignancies (1) and presents a substantial health problem, with an estimated 367,000 new cases diagnosed worldwide in 2015 and an associated 359,000 deaths in the same year (2). PDAC is currently the fourth highest cause of cancer death in developed countries and its five year survival is less than 5% while average survival is only 6–9 months after diagnosis (3-5), If outcomes are not improved, the disease is predicted to be the second leading cause of cancer-related mortality within the next decade, likely due to an aging population (6).
This bleak outlook for PDAC is predicated on several factors. The disease has an early and insidious dissemination, which is often due to non-specific or non-existent symptoms, a lack of sensitive and specific tumor markers, and difficulties in imaging early-stage tumors (7,8). The aggressive nature of PDAC leads to rapid invasion of local structures and early metastases, which leaves only 15–20% of patients as candidates for curative surgical resection (5). Even with surgical resection, PDAC 5-year survival only improves to 15–20% (9). PDAC is characterized by a remarkable resistance (or tolerance) to most conventional treatment options, including chemotherapy, radiotherapy and molecularly targeted therapy (10). PDAC harbors extensive genetic and epigenetic heterogeneity, not only among tumors from different individuals, but also within a single tumor and across metastatic sites from the same individual (11). Finally, PDAC has a complex and dense tumor microenvironment that is difficult to assemble and study, while also posing a significant barrier to treatment administration (12,13).
Significant advances in our understanding of PDAC have been made. Activating mutations in the KRAS oncogene appears to be the initiating event in the vast majority of PDAC. Studies have shown that activating KRAS mutations are uniquely sufficient to initiate premalignant lesions, termed pancreatic intraepithelial neoplasia (PanIN), in the exocrine pancreas (14). PanIN can progress to locally invasive and metastatic pancreatic cancer by way of stepwise mutations in tumor suppressor genes (15). Genetic alterations affecting CDKN2A, TP53 and SMAD4 cooperate with oncogenic KRAS to accelerate the progression of PDAC (16,17). Genome wide studies of PDAC have identified additional mutations and pathways that are crucial to the progression of PDAC (18,19). Other studies have demonstrated the importance of chromosomal alterations, ubiquitin proteases and transcription factor alterations that work in concert with KRAS mutations to drive PDAC forward (19-22). While our molecular knowledge of PDAC has rapidly progressed, the translation of this knowledge into relevant therapies has moved rather slowly.
Effective models of PDAC are absolutely critical to improving patient outcomes. Preclinical models provide a bridge to the clinic, a tool for developing strategies for early disease detection and are a requisite part of the drug development pipeline. However, these goals have remained frustratingly elusive, presumably due to our limited ability to reproduce critical in vivo features of the disease. Notably, our preclinical models struggle to reproduce the stromal microenvironment and the tumor interaction with the immune system. PDAC is characterized by a prominent fibrotic reaction with only small nests of adenocarcinoma cells; a number of studies provide compelling evidence that the stromal reaction plays a critical role in PDAC progression (23-25). The extensive fibrosis creates an environment characterized by severe hypoxia and nutrient deprivation (26,27). PDAC cells are adapted to survive in these conditions through various mechanisms, mainly driven by hypoxia-inducible transcription factor 1α (HIF1α) and oncogenic KRAS (28,29). The hypoxia and nutrient deprivation creates a climate conducive to further mutations and leads to PDAC’s characteristic heterogeneity (11,30). The excessive fibrosis also creates deficient vasculature, which makes drug delivery difficult (13,31,32). This makes treating PDAC more intricate because therapies have to target not only the cancer cells themselves but also the stroma (33). Highlighting the complexity of the stromal role in PDAC, several studies in murine PDAC models have shown that completely ablating the stroma paradoxically led to more aggressive tumor types and decreased overall survival, suggesting a protective role of stroma (34,35).
Preclinical models also struggle to fully recapitulate PDAC because of the intricate interaction between the fibrotic stroma and our immune system. Despite immune cell infiltration in PDAC, the immune system does not actively target the cancer as aggressively as would be expected, which suggests an immunosuppressive phenotype, even at the earliest stages of the disease (36,37). A growing body of evidence suggests that CD4+ regulatory T cells in the stroma play a crucial part in warding off the host immune response. This feature is clinically important because factors that mediate the suppression of active anti-tumor immunity, such as the ligand for programmed cell death protein 1 (PD-L1) expressed on cancer cells, form the basis of the current generation of immunotherapeutic approaches that have been studied in PDAC (38).
This divide between preclinical model responses to therapeutic agents and responses in the clinic has remained quite wide (13). Historically, preclinical testing has mostly occurred in vitro, in 2 dimensional (2D) cell culture assays, or in vivo, in either xenografts or animal models, including genetically engineered mouse models (GEMMs). More recently, hybrid systems where progenitor cells are cultured in 3D, called organoids, have emerged, combining the simplicity and controllability of in vitro culture with the possibility to reconstitute niches more similar to PDAC. Since pancreatic cells are epithelial cells that thrive in contact with other epithelial cells, this 3D architecture allows for these interactions to occur and provides the proper conditions to enable their polarization. In this review, we evaluate the advantages and disadvantages of our current preclinical models and discuss how these findings can be applied to translational studies for our patient’s benefit.
Human PDAC cell line
The first human PDAC cell line was established in 1963 (39) and since then many PDAC cell lines have been established and characterized via their unique molecular alterations and phenotypes (40). Studying cell lines provides several very practical advantages for studying PDAC. They are homogenous, easy to propagate and can grow indefinitely. These features allow for low-cost, easily replicable models that can screen essential genes, develop prognostic classifiers, predictive biomarkers and the development of novel anti-cancer drug targets (40).
While cell lines provide easy and rapidly replicable models of PDAC, these same features render them a less than optimal replication of in vivo PDAC. First, there are only a handful of well-defined cell lines currently available; therefore they do not represent the heterogeneous nature of PDAC (40-42). Indeed, expression profile studies of PDAC cell lines show significant differences between those seen in patient tumors or xenografts (43). Second, these cell lines select for mutations and phenotypes that advantage growth in a monolayer but are unlikely to be favored in vivo (44). The monolayer selection process advantages cancers that yield continuous cell lines, which tend to be the most aggressive, high stage and poorly differentiated tumors, leading to an underrepresentation of slow growing variants (42). The selection of aggressive clones means that these cell lines have already acquired the changes needed for the cells to grow as metastatic deposits in distant sites, rendering them inadequate to study cancer progression (45). At best, individual cancer cell lines provide a snapshot of the tumor at the time the biopsy was taken. This leads to therapies that only target the most aggressive clones, while sparing the majority of the tumor actually present in human PDAC (45). Thirdly, since these cell lines grow as monolayers, they lack the essential tumor microenvironment that leads to structural organization and functional differentiation of the tumor (46). Finally, the lack of an immune system ensures that mutations necessary for warding off the host immune system are significantly underrepresented.
All of these faults inherent in PDAC cell lines render them relevant only as a proof-of-principle preclinical model, making other models crucial for translating this information into possible therapies. Despite these many faults, the ability to grow and manipulate cell lines has allowed our group and others to leverage these characteristics to identify and study biomarkers for early disease detection. For example, cell lines can be grown in stable isotope labeled essential amino acids, a method termed stable isotope labeling by amino acids in cell culture (SILAC). In this way, the entire cellular proteome can be stably labeled for comparative proteomics. Our group has deeply explored this approach to interrogate human serum samples for disease specific protein biomarkers (47-51).
To identify and validate PDAC specific biomarkers, we have focused our efforts on studying the secreted proteome of disease specific cells. Beyond adenocarcinoma derived cell lines, we have also looked at tumor microenvironment derived cell lines. Pancreatic stellate cells (PSCs) are one of the major supportive cells of the exocrine pancreas. PSCs become activated in response to pancreatic injury and, more importantly, in PDAC (52,53). Upon activation, PSCs proliferate, lose the ability to store vitamin A, and express α-smooth muscle actin (α-SMA) and collagen I (53,54). It is in the activated state that PSCs play a major role in the pathogenesis of PDAC. Activated PSCs found in tumor desmoplasia that express α-SMA and collagen I are likely the major producers of the extracellular matrix seen in PDAC (54-59). We have characterized, created and SILAC labeled protein libraries consisting of the secreted proteomes of both PDAC (47) and activated PSC cell lines (60). We have demonstrated that these SILAC labeled proteomes can be used as internal standards for biomarker validation and monitoring using an innovative, multiplexed, mass spectrometry-based assay (48).
Furthermore, PSCs differentiate into tumor associated fibroblasts (TAFs), which a growing body of evidence suggests are the key drivers of stromal proliferation and chemoresistance, especially in PDAC (61). Normally, fibroblasts support healthy tissues via the secretion and remodeling of extracellular matrix. In PDAC, TAFs increase rates of proliferation, secrete proteins that activate survival, and, most importantly, promote chemoresistance (62). TAFs role in chemoresistance makes them a possible pharmacological target, which would promote greater tumor access for chemotherapy drugs by reducing surrounding stroma (63).
Cell line based xenograft
One potential solution to address many of the weaknesses of cell lines is to transplant cell lines into severe combined immunodeficient (SCID) murine models to create a cell line xenograft. These models can be made either subcutaneously or orthotopically (directly into the mouse pancreas). After injection, these xenografts recruit and synthesize their own stroma. Subcutaneous transplantation is favored for drug development by pharmaceutical companies because they are convenient, inexpensive, allow for rapid screening to assess safety and efficacy, and allow for easy assessment of tumor size. They form palpable tumor nodules within 2–6 weeks and are largely free of regulatory constraints. However, this is a less biologically faithful model. Orthotopic transplantation is clearly more reminiscent of human PDAC but this procedure is more costly and it is much more difficult to discern the response to a therapeutic agent without sacrificing the murine model (64). Xenografts have some predictive value and have helped prioritize compound testing, while showing more genetic diversity than cell lines grown as monolayers (65,66).
However, cell line based xenografts have significant weaknesses that limit their ability to predict therapeutic responses in clinical settings. Since the murine models in xenografts have to be immunocompromised, the tumors can develop without the selective pressure that an immune system normally places on PDAC (67). This makes it impossible to research immunotherapy in xenograft models. Additionally, SCID mice are more predisposed to double strand DNA breaks, giving them greater opportunities for mutations and a less robust response to cytotoxic agents than is seen in humans (68). Further limiting their clinical appeal, xenografts select for the most aggressive cancer clones causing them to grow as homogenous masses with limited stromal infiltration even though PDAC is a majority stromal microenvironment (33). Finally, xenografts are made from a limited number of cell lines and subsequently, fail to represent the great genetic and phenotypic diversity apparent in the human disease.
Some of these limitations can be overcome via CRISPR/Cas9 technology, which allows for the creation of syngeneic and humanized mice. Syngeneic/allograft transplant models are created by transplanting cancerous cells or solid tumors derived from the same genetic strain. This prevents transplant rejection by the host’s immune system so immunocompromising the model becomes unnecessary. This allows these models to be particularly efficacious in studying immunotherapies (69,70). The primary shortcoming of syngeneic mice is that the tumor cells are rodent and therefore do not completely recapitulate human PDAC (71). Humanized mice are immunodeficient mice with IL-2 receptor gamma chain mutations, which allows for the development of human immune systems following engraftment of hematopoietic stem cells (72). These mice are now used as in vivo models to study human hematopoiesis, immunity, regeneration, stem cell function, cancer, and human-specific infectious agents without putting patients at risk (72). However, humanized murine models are still limited since they cannot fully replicate the human immune system. They have limited lymph node development, HLA superfamilies, and inappropriate immune cell trafficking (73).
These deficiencies are readily apparent when studies have assessed the clinical effectiveness of therapies shown to have efficacy in cell line xenografts. An assessment by the NCI of evidence accumulated over several decades showed only moderate predictive value and even less correlation between data obtained from xenografts and clinical efficacy (66). Several prominent examples highlight the shortcomings of cell line xenograft models in clinical drug development. In 2000, Bruns et al. (74) found that the EGFR inhibitor cetuximab, in combination with gemcitabine, induced an 85% regression in a cell line xenograft model. However, when tested in phase III clinical trial, this treatment was shown to be ineffective (75). Another study found that the PPAR-gamma agonists thiazolidinediones (TZDs) had anti-tumor activity in xenografts, which was particularly exciting since TZDs have limited toxicity and are already approved as diabetic therapy by the FDA (76). In phase II clinical trials, TZDs were a clear failure as tumors in all patients rapidly progressed during the trial (77). The literature is littered with numerous other clinical trials that have had similar outcomes (65,78-81).
There are ways to improve the efficacy of xenografts such as a standardized definition of response (82) and a larger available repertoire of cell lines. Overall though, it seems that an improved mouse model which more closely resembles the human disease is needed for effective drug discovery.
Patient-derived tumor xenograft (PDX)
The PDX model was developed to address some of these shortcomings. While similar to cell line xenografts, PDXs are made by transplanting a large piece of a patient’s tumor, typically from a surgical resection specimen. One of the main advantages of PDXs is that when these surgical resections are removed, the stroma that surrounds and supports the cancer cells is transplanted as well. This allows PDXs to retain morphological characteristics of the original PDAC specimen as well as metastatic potential from the implantation site (83,84). Furthermore, the murine stroma is integrated into networks of expanding PDAC cells (85). Additionally, PDXs closely mirror responses in human patients to chemotherapeutic agents (86), possibly due to the carried over tumor stroma and replicated murine stroma (83,84,87). In fact, transcriptomic analysis of PDXs can predict the sensitivity to anticancer drugs and the clinical outcome of patients with PDAC (88). PDXs also have consistent biological properties and stable phenotypes across multiple passages (78), allowing for characterization of genetic mutations present in a specific tumor via genome sequencing and gene expression profiling, which may open up the possibility of personalized chemotherapeutic regimens (89). Our group and collaborators have shown that PDXs can be leveraged to generate and test gene expression models of chemotherapy response and resistance (90). Comparing PDXs with differential responses to chemotherapy drugs such as gemcitabine, specific genes and pathways can be identified and applied prospectively. In a clinical trial where such a model was applied prospectively to patient derived circulating tumor cells, survival benefit was seen in patients receiving chemotherapy regimens predicted to be effective (90).
Unfortunately, there are several drawbacks to the PDX model. Currently, successful engraftment of resected tumor specimens remains difficult and, ironically, successful engraftment may be a negative predictor of a patient’s outcome after surgical resection (91). One way to increase the chances of a successful transplantation is to obtain a large amount of tissue from surgically resected patients but only 15% of PDAC patients are surgical candidates (9), and, even in that small percentage, getting enough tissue is difficult, meaning this will not benefit the majority of patients. Creating PDXs can take up to 6 months and is also prohibitively expensive since it requires generation of secondary and tertiary carriers to effectively test potential agents (92,93). Waiting 6 months is simply untenable for most PDAC patients considering median survival after diagnosis is only 6–9 months (5). Further complicating matters, PDXs, while better than cell line xenografts, may not accurately represent the heterogeneity of PDAC since it has been shown that the more aggressive phenotypes are favored to grow within the murine model (78,91). Evolution occurs with each successive clonal generation, which genetically separates the transplanted tumor from the actual PDAC (94). One study compared the expression of 15 selected genes between primary tumors and PDXs from subcutaneous injections and found that only three genes showed statistically significant co-relations (92). Finally, although PDXs have advantages when compared to cell line xenografts, PDXs still do not fully replicate stromal proliferation of PDAC or the host immune response (95).
Despite their inherent limitations, PDXs have been shown to be useful for PDAC patients that have enough surgical tissue and are projected to live longer than six months (89). PDXs actually have upwards of an 80% predictive value for therapeutic agents in qualifying patients (78). However, until surgical techniques improve, PDXs only have limited utility for PDAC and, hence other preclinical models are necessary.
Genetically engineered mouse model (GEMM)
The GEMM is a model approach that helps to mitigate many of the shortcomings seen in PDX models. These mice are created by introducing specific gene mutations in oncogenes and/or tumor-suppressor genes that are important in human PDAC, thereby recapitulating PDAC in the mouse. This was first accomplished by introducing activating mutations into KRAS, expressed in a pancreas specific manner, which resulted in ductal lesions reminiscent of PanIN, thought to represent the precancerous lesions which can evolve into PDAC (96). The most robust and well described GEMM is the KPC mouse, which incorporates mutations in the oncogenic KRAS and tumor suppressor Trp53, both driven by a pancreas-specific Cre, the Pdx1-Cre transgene, which is expressed in all cells of the pancreas from an early stage of embryonic development (97). Such autochthonous models recapitulate many of the features of the human disease and have confirmed causative roles for many mutant genes previously identified by human PDAC sequencing efforts. GEMMs have become the standard method to query the effect of a particular genetic mutation on PDAC progression. GEMMs exhibit many of the symptoms that define the human disease, such as pain and cachexia (98,99). GEMMs have been leveraged to study predisposing risk factors suspected in the human disease, such as obesity, a high calorie/high fat diet and chronic pancreatitis, all of which accelerate the development of PDAC in GEMMs (15,100). These similarities have also shown practical applications in drug discovery. For instance, the KPC model has deficient vasculature and dense stroma that decrease the delivery of anti-proliferative agents (13,26,31,32). These properties of the KPC model may explain the resistance to therapeutic agents similar to what is seen in the human disease (13). The advent of GEMMs has led to remarkable strides in our understanding of PDAC pathogenesis and provides an excellent model to investigate novel therapies. This has led to new therapeutic targets such as the autophagy, MEK, PI3K and Notch pathways (101-103). GEMMs have allowed researchers to discover the delicate balance between pro-malignant and restraining properties of the tumor stroma (34,35). Another advantage compared to xenograft models is GEMMs intact immune system, making it a useful tool to study the immune response in PDAC and to test novel immunotherapeutic compounds.
Since GEMMs such as the KPC model recapitulate the development of PDAC, progressing first through PanIN, they represent a promising tool for identifying biomarkers of early disease. Multiple proteomic studies have been performed to date, with several promising candidate biomarkers identified (104,105), although they remain to be successfully validated. With improved proteomic techniques and instruments now available, a repeat study of these models is warranted. More recently, glypican-1 expressing exosomes were identified in both PDAC cell lines and GEMMs, with promising results as a candidate biomarker for early detection in human blood (106). Validation of this innovative biomarker is eagerly awaited.
While the development of GEMMs was a pivotal innovation in preclinical PDAC research, significant weaknesses have been identified. GEMMs are expensive and time consuming (20). Attempting to accelerate the development process by introducing multiple genetic alterations at once comes at the cost of making GEMMs a less faithful model for sporadic, non-inherited PDAC. While the extensive stromal component increases the efficacy of preclinical therapeutic trials, the overall lack of neoplastic cellularity makes it difficult to isolate and characterize the malignant cells in murine PDAC (107). Overcoming this problem requires expensive imaging equipment that is not readily available to most labs, which makes them significantly more expensive than cell lines or xenografts. Furthermore, despite having better physiologic overlap with human PDAC than xenografts, there are still significant differences between murine and human malignancies. For instance, p53 and BRCA1 are on the same chromosome in mice, which increases the odds of concomitant deletion (68). Mice also have different telomere properties than humans, which leads to a different progression of mutations not seen in human PDAC (108). These differences between mice and humans are underscored by the failure of a promising hedgehog pathway inhibitor, initially characterized to be effective in the KPC GEMM (13), but a subsequent clinical trial did not confirm these findings. Therefore, investigating other preclinical models that can accurately predict treatment response of the human disease remains a clear and unmet need.
Organoid
As previously discussed, growing cells in two dimensional culture results in vastly different genetic expression compared to those grown in 3D (109-111). The added third dimension exponentially increases the number of cell-to-cell interactions and more closely resembles how cells organize in vivo. Recently, the development of innovative organoid approaches has generated great interest. Organoids are 3D structures derived from either pluripotent stem cells, neonatal tissue stem cells or adult-derived stem/progenitor cells, in which cells spontaneously self-organize into structures that resemble the in vivo tissue in terms of cellular composition and tissue function (112). Normal or malignant pancreatic ductal cells are embedded in Matrigel, which contains critical components of basement membrane, along with growth factor components such as EGF (mitogen), R-spondin-1 (enhances Wnt signalling), Noggin (inhibits BMP signalling), Wnt3a FGF10 (mitogen), nicotinamide, A83-01 (Alk inhibitor) and prostaglandin E2 (PGE2, mitogen).
In addition to murine derived organoids, our group has developed an approach to derive organoids from human normal and malignant pancreatic ductal cells (107). Human derived organoids can be established at a high rate from small amounts of tissue, such as a fine needle biopsy. Human derived PDAC organoids possess the mutational complexity found in the human disease, and clonal heterogeneity is maintained even after numerous passages as determined by single cell copy number analysis (personal correspondence). Human and murine derived organoids can be orthotopically transplanted into mice and recapitulate many of the features of the human disease. Unlike xenografts, organoid derived orthotopic tumors form abundant collagen deposition characteristic of PDAC in vivo and in GEMMs (13,107). Normal pancreatic cells, paraneoplastic cells, and neoplastic pancreatic cells are able to grow equally well, which is in contrast to the favored growth of neoplastic cells seen in xenografts and cell lines (113).
One main advantage of organoids is they allow the comparison of normal pancreatic cells, preneoplastic cells, and PDAC cells due to multiple cultures that are rapidly visible compared to excising specimens from murine models. They provide opportunities to observe and evaluate the disease progression unlike xenografts models that simply repopulate as malignancies in the murine pancreas. Organoids permit more thorough molecular assessment of PDAC via DNA, RNA and protein based assays (113).
Though the organoid model was only recent developed, first described in PDAC in 2015, several studies have already been published demonstrating how organoids can be leveraged to study important biological questions, such as the components of the tumor microenvironment (61), the role of neuronal signaling (114), and the role of redox regulation (115). For instance, organoid cultures have implicated particular subpopulations of TAFs located immediately adjacent to PDAC tissue that produced desmoplastic stroma (61).
Organoids can be grown from surgical resections and fine needle aspirations, which greatly expands the patient pool that can generate models of their PDAC compared to xenograft models. Research is currently being conducted to isolate malignant PDAC cells from patients’ blood samples. This would allow the study of the unique mutations and adaptations that cause metastasis which currently remain a mystery. This would also allow for easier sampling of patient tumors without requiring fine needle assays, thus decreasing expensive and invasiveness of sampling. Organoids can also better preserve PDAC cell heterogeneity than other preclinical models by recapitulating stem cells. Possible alterations in plasticity and epigenetics that are only observed in a 3D matrix are now possible to study. Organoids can also create Pan-IN-like structures, which may lead to the development of reliable tumor markers that can detect the cancer before it can enter its rapidly invasive stages. Ultimately, organoids may allow the collection and culturing of enough patient samples to test the responsiveness of an individual patient’s cancer’s susceptibility to numerous chemotherapeutic and novel agents in a high-throughput fashion, similar to testing bacterial culture susceptibility to particular antibiotics. Validation for such an approach is ongoing (ClinicalTrials.gov Identifier NCT03033927). This model remains early in its characterization and further study is needed to fully understand both strengths and weaknesses of this approach.
Conclusions
We now possess a wide variety of PDAC models for studying disease and therapy, all with model-specific strengths and weaknesses (see Table 1). Choice of model should be made carefully based on purpose of the study and the question that the investigator is attempting to answer. Similarly, while reviewing results of studies utilizing each of these models, the same strengths and weaknesses should be weighed to put these studies in context. New and innovative models continue to be developed which may further move the field forward. Examples include GEMMs with inducible genetic lesions, allowing for genes, such as KRAS to be turned on and off (116), and organoid coculture models which integrate stromal and immune components (61). Expanded use of current models and those in development are likely to lead to greater understanding of disease biology, identification of clinically useful biomarkers of early disease and the development of new and more effective therapies in this challenging disease.
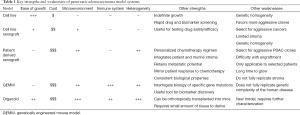
Full table
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Feldmann G, Maitra A. Molecular genetics of pancreatic ductal adenocarcinomas and recent implications for translational efforts. J Mol Diagn 2008;10:111-22. [Crossref] [PubMed]
- Ferlay J, Soerjomataram I, Dikshit R, et al. Cancer incidence and mortality worldwide: sources, methods and major patterns in GLOBOCAN 2012. Int J Cancer 2015;136:E359-86. [Crossref] [PubMed]
- Rahib L, Smith BD, Aizenberg R, et al. Projecting cancer incidence and deaths to 2030: the unexpected burden of thyroid, liver, and pancreas cancers in the United States. Cancer Res 2014;74:2913-21. [Crossref] [PubMed]
- Hidalgo M. Pancreatic cancer. N Engl J Med 2010;362:1605-17. [Crossref] [PubMed]
- Ryan DP, Hong TS, Bardeesy N. Pancreatic adenocarcinoma. N Engl J Med 2014;371:2140-1. [Crossref] [PubMed]
- Malvezzi M, Bertuccio P, Rosso T, et al. European cancer mortality predictions for the year 2015: does lung cancer have the highest death rate in EU women? Ann Oncol 2015;26:779-86. [Crossref] [PubMed]
- Hezel AF, Kimmelman AC, Stanger BZ, et al. Genetics and biology of pancreatic ductal adenocarcinoma. Genes Dev 2006;20:1218-49. [Crossref] [PubMed]
- Siegel RL, Miller KD, Jemal A. Cancer statistics, 2015. CA Cancer J Clin 2015;65:5-29. [Crossref] [PubMed]
- He J, Ahuja N, Makary MA, et al. 2564 resected periampullary adenocarcinomas at a single institution: trends over three decades. HPB (Oxford) 2014;16:83-90. [Crossref] [PubMed]
- Abbruzzese JL, Hess KR. New option for the initial management of metastatic pancreatic cancer? J Clin Oncol 2014;32:2405-7. [Crossref] [PubMed]
- Jones S, Zhang X, Parsons DW, et al. Core signaling pathways in human pancreatic cancers revealed by global genomic analyses. Science 2008;321:1801-6. [Crossref] [PubMed]
- Adler G. Has the biology and treatment of pancreatic diseases evolved? Best Pract Res Clin Gastroenterol 2004;18 Suppl:83-90. [Crossref] [PubMed]
- Olive KP, Jacobetz MA, Davidson CJ, et al. Inhibition of Hedgehog signaling enhances delivery of chemotherapy in a mouse model of pancreatic cancer. Science 2009;324:1457-61. [Crossref] [PubMed]
- Kanda M, Matthaei H, Wu J, et al. Presence of somatic mutations in most early-stage pancreatic intraepithelial neoplasia. Gastroenterology 2012;142:730-3.e9. [Crossref] [PubMed]
- Guerra C, Schuhmacher AJ, Canamero M, et al. Chronic pancreatitis is essential for induction of pancreatic ductal adenocarcinoma by K-Ras oncogenes in adult mice. Cancer Cell 2007;11:291-302. [Crossref] [PubMed]
- Morris JP, Wang SC, Hebrok M. KRAS, Hedgehog, Wnt and the twisted developmental biology of pancreatic ductal adenocarcinoma. Nat Rev Cancer 2010;10:683-95. [Crossref] [PubMed]
- Yachida S, White CM, Naito Y, et al. Clinical significance of the genetic landscape of pancreatic cancer and implications for identification of potential long-term survivors. Clin Cancer Res 2012;18:6339-47. [Crossref] [PubMed]
- Waddell N, Pajic M, Patch AM, et al. Whole genomes redefine the mutational landscape of pancreatic cancer. Nature 2015;518:495-501. [Crossref] [PubMed]
- Biankin AV, Waddell N, Kassahn KS, et al. Pancreatic cancer genomes reveal aberrations in axon guidance pathway genes. Nature 2012;491:399-405. [Crossref] [PubMed]
- Pérez-Mancera PA, Rust AG, van der Weyden L, et al. The deubiquitinase USP9X suppresses pancreatic ductal adenocarcinoma. Nature 2012;486:266-70. [PubMed]
- Mann KM, Ward JM, Yew CC, et al. Sleeping Beauty mutagenesis reveals cooperating mutations and pathways in pancreatic adenocarcinoma. Proc Natl Acad Sci U S A 2012;109:5934-41. [Crossref] [PubMed]
- Rad R, Rad L, Wang W, et al. A conditional piggyBac transposition system for genetic screening in mice identifies oncogenic networks in pancreatic cancer. Nat Genet 2015;47:47-56. [Crossref] [PubMed]
- Hwang RF, Moore T, Arumugam T, et al. Cancer-associated stromal fibroblasts promote pancreatic tumor progression. Cancer Res 2008;68:918-26. [Crossref] [PubMed]
- Vonlaufen A, Joshi S, Qu C, et al. Pancreatic stellate cells: partners in crime with pancreatic cancer cells. Cancer Res 2008;68:2085-93. [Crossref] [PubMed]
- Lonardo E, Frias-Aldeguer J, Hermann PC, et al. Pancreatic stellate cells form a niche for cancer stem cells and promote their self-renewal and invasiveness. Cell Cycle 2012;11:1282-90. [Crossref] [PubMed]
- Erkan M, Reiser-Erkan C, Michalski CW, et al. Cancer-stellate cell interactions perpetuate the hypoxia-fibrosis cycle in pancreatic ductal adenocarcinoma. Neoplasia 2009;11:497-508. [Crossref] [PubMed]
- Kong B, Cheng T, Wu W, et al. Hypoxia-induced endoplasmic reticulum stress characterizes a necrotic phenotype of pancreatic cancer. Oncotarget 2015;6:32154-60. [PubMed]
- Schönenberger MJ, Kovacs WJ. Hypoxia signaling pathways: modulators of oxygen-related organelles. Front Cell Dev Biol 2015;3:42. [Crossref] [PubMed]
- Ye LY, Zhang Q, Bai XL, et al. Hypoxia-inducible factor 1alpha expression and its clinical significance in pancreatic cancer: a meta-analysis. Pancreatology 2014;14:391-7. [Crossref] [PubMed]
- Dauer P, Nomura A, Saluja A, et al. Microenvironment in determining chemo-resistance in pancreatic cancer: Neighborhood matters. Pancreatology 2017;17:7-12. [Crossref] [PubMed]
- Jacobetz MA, Chan DS, Neesse A, et al. Hyaluronan impairs vascular function and drug delivery in a mouse model of pancreatic cancer. Gut 2013;62:112-20. [Crossref] [PubMed]
- Provenzano PP, Cuevas C, Chang AE, et al. Enzymatic targeting of the stroma ablates physical barriers to treatment of pancreatic ductal adenocarcinoma. Cancer Cell 2012;21:418-29. [Crossref] [PubMed]
- Feig C, Gopinathan A, Neesse A, et al. The pancreas cancer microenvironment. Clin Cancer Res 2012;18:4266-76. [Crossref] [PubMed]
- Rhim AD, Oberstein PE, Thomas DH, et al. Stromal elements act to restrain, rather than support, pancreatic ductal adenocarcinoma. Cancer Cell 2014;25:735-47. [Crossref] [PubMed]
- Özdemir BC, Pentcheva-Hoang T, Carstens JL, et al. Depletion of carcinoma-associated fibroblasts and fibrosis induces immunosuppression and accelerates pancreas cancer with reduced survival. Cancer Cell 2014;25:719-34. [Crossref] [PubMed]
- Inman KS, Francis AA, Murray NR. Complex role for the immune system in initiation and progression of pancreatic cancer. World J Gastroenterol 2014;20:11160-81. [Crossref] [PubMed]
- Amedei A, Niccolai E, Prisco D. Pancreatic cancer: role of the immune system in cancer progression and vaccine-based immunotherapy. Hum Vaccin Immunother 2014;10:3354-68. [Crossref] [PubMed]
- Lutz ER, Wu AA, Bigelow E, et al. Immunotherapy converts nonimmunogenic pancreatic tumors into immunogenic foci of immune regulation. Cancer Immunol Res 2014;2:616-31. [Crossref] [PubMed]
- Dobrynin YV. Establishment and Characteristics of Cell Strains from Some Epithelial Tumors of Human Origin. J Natl Cancer Inst 1963;31:1173-95. [PubMed]
- Deer EL, Gonzalez-Hernandez J, Coursen JD, et al. Phenotype and genotype of pancreatic cancer cell lines. Pancreas 2010;39:425-35. [Crossref] [PubMed]
- Rückert F, Aust D, Bohme I, et al. Five primary human pancreatic adenocarcinoma cell lines established by the outgrowth method. J Surg Res 2012;172:29-39. [Crossref] [PubMed]
- Gillet JP, Varma S, Gottesman MM. The clinical relevance of cancer cell lines. J Natl Cancer Inst 2013;105:452-8. [Crossref] [PubMed]
- Gadaleta E, Cutts RJ, Kelly GP, et al. A global insight into a cancer transcriptional space using pancreatic data: importance, findings and flaws. Nucleic Acids Res 2011;39:7900-7. [Crossref] [PubMed]
- Froeling FE, Marshall JF, Kocher HM. Pancreatic cancer organotypic cultures. J Biotechnol 2010;148:16-23. [Crossref] [PubMed]
- Masters JR. Human cancer cell lines: fact and fantasy. Nat Rev Mol Cell Biol 2000;1:233-6. [Crossref] [PubMed]
- Fidler IJ. The pathogenesis of cancer metastasis: the 'seed and soil' hypothesis revisited. Nat Rev Cancer 2003;3:453-8. [Crossref] [PubMed]
- Yu KH, Barry CG, Austin D, et al. Stable isotope dilution multidimensional liquid chromatography-tandem mass spectrometry for pancreatic cancer serum biomarker discovery. J Proteome Res 2009;8:1565-76. [Crossref] [PubMed]
- Wehr AY, Hwang WT, Blair IA, et al. Relative Quantification of Serum Proteins from Pancreatic Ductal Adenocarcinoma Patients by Stable Isotope Dilution Liquid Chromatography-Mass Spectrometry. J Proteome Res 2012;11:1749-58. [Crossref] [PubMed]
- Rangiah K, Tippornwong M, Sangar V, et al. Differential Secreted Proteome Approach in Murine Model for Candidate Biomarker Discovery in Colon Cancer. J Proteome Res 2009;8:5153-64. [Crossref] [PubMed]
- Yan Y, Weaver VM, Blair IA. Analysis of protein expression during oxidative stress in breast epithelial cells using a stable isotope labeled proteome internal standard. J Proteome Res 2005;4:2007-14. [Crossref] [PubMed]
- Shah SJ, Yu KH, Sangar V, et al. Identification and Quantification of Preterm Birth Biomarkers in Human Cervicovaginal Fluid by Liquid Chromatography/Tandem Mass Spectrometry. J Proteome Res 2009;8:2407-17. [Crossref] [PubMed]
- Apte MV, Haber PS, Applegate TL, et al. Periacinar stellate shaped cells in rat pancreas: identification, isolation, and culture. Gut 1998;43:128-33. [Crossref] [PubMed]
- Bachem MG, Schneider E, Gross H, et al. Identification, culture, and characterization of pancreatic stellate cells in rats and humans. Gastroenterology 1998;115:421-32. [Crossref] [PubMed]
- Apte MV, Park S, Phillips PA, et al. Desmoplastic reaction in pancreatic cancer: role of pancreatic stellate cells. Pancreas 2004;29:179-87. [Crossref] [PubMed]
- Yen TW, Aardal NP, Bronner MP, et al. Myofibroblasts are responsible for the desmoplastic reaction surrounding human pancreatic carcinomas. Surgery 2002;131:129-34. [Crossref] [PubMed]
- Armstrong T, Packham G, Murphy LB, et al. Type I collagen promotes the malignant phenotype of pancreatic ductal adenocarcinoma. Clin Cancer Res 2004;10:7427-37. [Crossref] [PubMed]
- Binkley CE, Zhang L, Greenson JK, et al. The molecular basis of pancreatic fibrosis: common stromal gene expression in chronic pancreatitis and pancreatic adenocarcinoma. Pancreas 2004;29:254-63. [Crossref] [PubMed]
- Köninger J, Giese T, di Mola FF, et al. Pancreatic tumor cells influence the composition of the extracellular matrix. Biochem Biophys Res Commun 2004;322:943-9. [Crossref] [PubMed]
- Yoshida S, Yokota T, Ujiki M, et al. Pancreatic cancer stimulates pancreatic stellate cell proliferation and TIMP-1 production through the MAP kinase pathway. Biochem Biophys Res Commun 2004;323:1241-5. [Crossref] [PubMed]
- Wehr AY, Furth EE, Sangar V, et al. Analysis of the human pancreatic stellate cell secreted proteome. Pancreas 2011;40:557-66. [Crossref] [PubMed]
- Öhlund D, Handly-Santana A, Biffi G, et al. Distinct populations of inflammatory fibroblasts and myofibroblasts in pancreatic cancer. J Exp Med 2017;214:579-96. [PubMed]
- Cirri P, Chiarugi P. Cancer associated fibroblasts: the dark side of the coin. Am J Cancer Res 2011;1:482-97. [PubMed]
- Duluc C, Moatassim-Billah S, Chalabi-Dchar M, et al. Pharmacological targeting of the protein synthesis mTOR/4E-BP1 pathway in cancer-associated fibroblasts abrogates pancreatic tumour chemoresistance. EMBO Mol Med 2015;7:735-53. [Crossref] [PubMed]
- Walters DM, Stokes JB, Adair SJ, et al. Clinical, molecular and genetic validation of a murine orthotopic xenograft model of pancreatic adenocarcinoma using fresh human specimens. PLoS One 2013;8:e77065. [Crossref] [PubMed]
- Voskoglou-Nomikos T, Pater JL, Seymour L. Clinical predictive value of the in vitro cell line, human xenograft, and mouse allograft preclinical cancer models. Clin Cancer Res 2003;9:4227-39. [PubMed]
- Johnson JI, Decker S, Zaharevitz D, et al. Relationships between drug activity in NCI preclinical in vitro and in vivo models and early clinical trials. Br J Cancer 2001;84:1424-31. [Crossref] [PubMed]
- Frese KK, Tuveson DA. Maximizing mouse cancer models. Nat Rev Cancer 2007;7:645-58. [Crossref] [PubMed]
- Sharpless NE, DePinho RA. The mighty mouse: genetically engineered mouse models in cancer drug development. Nat Rev Drug Discov 2006;5:741-54. [Crossref] [PubMed]
- Klein C, Waldhauer I, Nicolini VG, et al. Cergutuzumab amunaleukin (CEA-IL2v), a CEA-targeted IL-2 variant-based immunocytokine for combination cancer immunotherapy: Overcoming limitations of aldesleukin and conventional IL-2-based immunocytokines. Oncoimmunology 2017;6:e1277306. [Crossref] [PubMed]
- Labrijn AF, Meesters JI, Bunce M, et al. Efficient Generation of Bispecific Murine Antibodies for Pre-Clinical Investigations in Syngeneic Rodent Models. Sci Rep 2017;7:2476. [Crossref] [PubMed]
- Murphy JF. Pre-Clinical Murine Models: Syngeneic Models for Immuno-Oncology. MOJ Immunol 2015;2:4. [Crossref]
- Brehm MA, Shultz LD, Greiner DL. Humanized mouse models to study human diseases. Curr Opin Endocrinol Diabetes Obes 2010;17:120-5. [Crossref] [PubMed]
- Shultz LD, Brehm MA, Garcia-Martinez JV, et al. Humanized mice for immune system investigation: progress, promise and challenges. Nat Rev Immunol 2012;12:786-98. [Crossref] [PubMed]
- Bruns CJ, Harbison MT, Davis DW, et al. Epidermal growth factor receptor blockade with C225 plus gemcitabine results in regression of human pancreatic carcinoma growing orthotopically in nude mice by antiangiogenic mechanisms. Clin Cancer Res 2000;6:1936-48. [PubMed]
- Philip PA, Benedetti J, Corless CL, et al. Phase III study comparing gemcitabine plus cetuximab versus gemcitabine in patients with advanced pancreatic adenocarcinoma: Southwest Oncology Group-directed intergroup trial S0205. J Clin Oncol 2010;28:3605-10. [Crossref] [PubMed]
- Sarraf P, Mueller E, Jones D, et al. Differentiation and reversal of malignant changes in colon cancer through PPARgamma. Nat Med 1998;4:1046-52. [Crossref] [PubMed]
- Kulke MH, Demetri GD, Sharpless NE, et al. A phase II study of troglitazone, an activator of the PPARgamma receptor, in patients with chemotherapy-resistant metastatic colorectal cancer. Cancer J 2002;8:395-9. [Crossref] [PubMed]
- Aparicio S, Hidalgo M, Kung AL. Examining the utility of patient-derived xenograft mouse models. Nat Rev Cancer 2015;15:311-6. [Crossref] [PubMed]
- Van Cutsem E, van de Velde H, Karasek P, et al. Phase III trial of gemcitabine plus tipifarnib compared with gemcitabine plus placebo in advanced pancreatic cancer. J Clin Oncol 2004;22:1430-8. [Crossref] [PubMed]
- End DW, Smets G, Todd AV, et al. Characterization of the antitumor effects of the selective farnesyl protein transferase inhibitor R115777 in vivo and in vitro. Cancer Res 2001;61:131-7. [PubMed]
- Thomas JP, Arzoomanian RZ, Alberti D, et al. Phase I pharmacokinetic and pharmacodynamic study of recombinant human endostatin in patients with advanced solid tumors. J Clin Oncol 2003;21:223-31. [Crossref] [PubMed]
- Sausville EA, Burger AM. Contributions of human tumor xenografts to anticancer drug development. Cancer Res 2006;66:3351-4, discussion 4. [Crossref] [PubMed]
- Fu X, Guadagni F, Hoffman RM. A metastatic nude-mouse model of human pancreatic cancer constructed orthotopically with histologically intact patient specimens. Proc Natl Acad Sci U S A 1992;89:5645-9. [Crossref] [PubMed]
- Loukopoulos P, Kanetaka K, Takamura M, et al. Orthotopic transplantation models of pancreatic adenocarcinoma derived from cell lines and primary tumors and displaying varying metastatic activity. Pancreas 2004;29:193-203. [Crossref] [PubMed]
- Delitto D, Pham K, Vlada AC, et al. Patient-derived xenograft models for pancreatic adenocarcinoma demonstrate retention of tumor morphology through incorporation of murine stromal elements. Am J Pathol 2015;185:1297-303. [Crossref] [PubMed]
- Garber K. From human to mouse and back: 'tumorgraft' models surge in popularity. J Natl Cancer Inst 2009;101:6-8. [Crossref] [PubMed]
- Rubio-Viqueira B, Hidalgo M. Direct in vivo xenograft tumor model for predicting chemotherapeutic drug response in cancer patients. Clin Pharmacol Ther 2009;85:217-21. [Crossref] [PubMed]
- Duconseil P, Gilabert M, Gayet O, et al. Transcriptomic analysis predicts survival and sensitivity to anticancer drugs of patients with a pancreatic adenocarcinoma. Am J Pathol 2015;185:1022-32. [Crossref] [PubMed]
- Hidalgo M, Bruckheimer E, Rajeshkumar NV, et al. A pilot clinical study of treatment guided by personalized tumorgrafts in patients with advanced cancer. Mol Cancer Ther 2011;10:1311-6. [Crossref] [PubMed]
- Yu KH, Ricigliano M, Hidalgo M, et al. Pharmacogenomic modeling of circulating tumor and invasive cells for prediction of chemotherapy response and resistance in pancreatic cancer. Clin Cancer Res 2014;20:5281-9. [Crossref] [PubMed]
- Garrido-Laguna I, Uson M, Rajeshkumar NV, et al. Tumor engraftment in nude mice and enrichment in stroma- related gene pathways predict poor survival and resistance to gemcitabine in patients with pancreatic cancer. Clinical cancer research: an official journal of the American Association for Cancer Research 2011;17:5793-800.
- Rubio-Viqueira B, Jimeno A, Cusatis G, et al. An in vivo platform for translational drug development in pancreatic cancer. Clin Cancer Res 2006;12:4652-61. [Crossref] [PubMed]
- Kim MP, Evans DB, Wang H, et al. Generation of orthotopic and heterotopic human pancreatic cancer xenografts in immunodeficient mice. Nat Protoc 2009;4:1670-80. [Crossref] [PubMed]
- Tentler JJ, Tan AC, Weekes CD, et al. Patient-derived tumour xenografts as models for oncology drug development. Nat Rev Clin Oncol 2012;9:338-50. [Crossref] [PubMed]
- Yachida S, Jones S, Bozic I, et al. Distant metastasis occurs late during the genetic evolution of pancreatic cancer. Nature 2010;467:1114-7. [Crossref] [PubMed]
- Aguirre AJ, Bardeesy N, Sinha M, et al. Activated Kras and Ink4a/Arf deficiency cooperate to produce metastatic pancreatic ductal adenocarcinoma. Genes Dev 2003;17:3112-26. [Crossref] [PubMed]
- Hingorani SR, Wang L, Multani AS, et al. Trp53R172H and KrasG12D cooperate to promote chromosomal instability and widely metastatic pancreatic ductal adenocarcinoma in mice. Cancer Cell 2005;7:469-83. [Crossref] [PubMed]
- Stopczynski RE, Normolle DP, Hartman DJ, et al. Neuroplastic changes occur early in the development of pancreatic ductal adenocarcinoma. Cancer Res 2014;74:1718-27. [Crossref] [PubMed]
- Gilabert M, Calvo E, Airoldi A, et al. Pancreatic cancer-induced cachexia is Jak2-dependent in mice. J Cell Physiol 2014;229:1437-43. [Crossref] [PubMed]
- Dawson DW, Hertzer K, Moro A, et al. High-fat, high-calorie diet promotes early pancreatic neoplasia in the conditional KrasG12D mouse model. Cancer Prev Res (Phila) 2013;6:1064-73. [Crossref] [PubMed]
- Yang S, Wang X, Contino G, et al. Pancreatic cancers require autophagy for tumor growth. Genes Dev 2011;25:717-29. [Crossref] [PubMed]
- Alagesan B, Contino G, Guimaraes AR, et al. Combined MEK and PI3K inhibition in a mouse model of pancreatic cancer. Clin Cancer Res 2015;21:396-404. [Crossref] [PubMed]
- Cook N, Frese KK, Bapiro TE, et al. Gamma secretase inhibition promotes hypoxic necrosis in mouse pancreatic ductal adenocarcinoma. J Exp Med 2012;209:437-44. [Crossref] [PubMed]
- Faca VM, Song KS, Wang H, et al. A mouse to human search for plasma proteome changes associated with pancreatic tumor development. PLoS Med 2008;5:e123. [Crossref] [PubMed]
- Menon R, Zhang Q, Zhang Y, et al. Identification of novel alternative splice isoforms of circulating proteins in a mouse model of human pancreatic cancer. Cancer Res 2009;69:300-9. [Crossref] [PubMed]
- Melo SA, Luecke LB, Kahlert C, et al. Glypican-1 identifies cancer exosomes and detects early pancreatic cancer. Nature 2015;523:177-82. [Crossref] [PubMed]
- Boj SF, Hwang C-I, Baker LA, et al. Organoid Models of Human and Mouse Ductal Pancreatic Cancer. Cell 2015;160:324-38. [Crossref] [PubMed]
- Artandi SE, Chang S, Lee SL, et al. Telomere dysfunction promotes non-reciprocal translocations and epithelial cancers in mice. Nature 2000;406:641-5. [Crossref] [PubMed]
- Zschenker O, Streichert T, Hehlgans S, et al. Genome-wide gene expression analysis in cancer cells reveals 3D growth to affect ECM and processes associated with cell adhesion but not DNA repair. PLoS One 2012;7:e34279. [Crossref] [PubMed]
- Ghosh S, Spagnoli GC, Martin I, et al. Three-dimensional culture of melanoma cells profoundly affects gene expression profile: a high density oligonucleotide array study. J Cell Physiol 2005;204:522-31. [Crossref] [PubMed]
- Ridky TW, Chow JM, Wong DJ, et al. Invasive three-dimensional organotypic neoplasia from multiple normal human epithelia. Nat Med 2010;16:1450-5. [Crossref] [PubMed]
- Huch M, Koo BK. Modeling mouse and human development using organoid cultures. Development 2015;142:3113-25. [Crossref] [PubMed]
- Huch M, Bonfanti P, Boj SF, et al. Unlimited in vitro expansion of adult bi-potent pancreas progenitors through the Lgr5/R-spondin axis. EMBO J 2013;32:2708-21. [Crossref] [PubMed]
- Sinha S, Fu YY, Grimont A, et al. PanIN neuroendocrine cells promote tumorigenesis via neuronal crosstalk. Cancer Res 2017;77:1868-79. [Crossref] [PubMed]
- Chio II, Jafarnejad SM, Ponz-Sarvise M, et al. NRF2 Promotes Tumor Maintenance by Modulating mRNA Translation in Pancreatic Cancer. Cell 2016;166:963-76. [Crossref] [PubMed]
- Ying H, Kimmelman AC, Lyssiotis CA, et al. Oncogenic Kras maintains pancreatic tumors through regulation of anabolic glucose metabolism. Cell 2012;149:656-70. [Crossref] [PubMed]


