Abstract
Circulating tumour cells (CTC) and tumour-related methylated DNA in blood have been separately assessed for their utility as a marker for subclinical metastasis in breast cancer. However, no studies have looked into the relation between the both molecular markers in this type of cancer. In this study, we investigated the correlations between total/methylated DNA and CTC in the blood from metastatic breast cancer patients. We simultaneously obtained whole blood, plasma and serum samples from 80 patients and 20 controls. The CellSearch System was used to enumerate CTC in blood samples. Plasma total DNA levels were determined by a QPCR method. Sera were analysed by methylation-specific QPCR for three markers: adenomatous polyposis coli (APC), ras association domain family protein 1A (RASSF1A) and oestrogen receptor 1 (ESR1). Total DNA levels in patients were significantly increased when compared with controls (P<0.001) and correlated with the number of CTC (r=0.418, P<0.001). Hypermethylation of one or more genes was detected in 42 (53%) serum samples from breast cancer patients and in three (16%) serum samples from controls (P=0.003). APC was hypermethylated in 29%, RASSF1A in 35% and ESR1 in 20% of breast cancer cases. Detection of a methylated gene in serum was associated with the detection of CTC in blood (P=0.03). The detection of large amounts of circulating total/methylated DNA correlated with the presence of CTC in the blood from patients with breast cancer. This can be interpreted in two ways: (a) CTC are a potential source of circulating tumour-specific DNA; (b) high numbers of CTC and circulating methylated DNA are both a phenotypic feature of more aggressive tumour biology.
Similar content being viewed by others
Main
Distant metastasis is the leading cause of cancer-related death in breast cancer, but early spread of tumour cells usually remains undetected even by high-resolution imaging technologies. With the use of traditional prognostic factors, it is still not possible to reliably identify those breast cancer patients who will eventually relapse with metastatic disease and are in need of adjuvant therapy. Therefore, the development of new molecular staging methods enabling individual risk assessment is of utmost importance. As haematogenous dissemination of tumour cells is the main mechanism for distant metastasis, the assessment of cancer patients' blood may be a highly desirable approach for detecting systemic tumour cell spreading (Pantel et al, 1999).
Several studies have suggested that the presence of circulating tumour cells (CTC) in patients' bone marrow or blood represents a promising marker for current risk classification systems for breast cancer. Recently, we showed that the presence of CK19+ disseminated tumour cells in the bone marrow by reverse transcriptase–PCR is an independent prognostic factor in untreated patients with breast cancer (Benoy et al, 2006). Moreover, a pooled analysis involving 4703 patients indicated that the presence of micrometastasis in the bone marrow at the time of diagnosis of breast cancer is an independent predictor of poor prognosis (Braun et al, 2005). CTC detection by the CellSearch System (Veridex LLC, Warren, NJ, USA), developed to automatically enrich and immunocytochemically detect CTC from peripheral blood, has been shown to provide significant prognostic information for patients with metastatic breast cancer starting first-line therapy (Cristofanilli et al, 2004, 2005). In latter studies, the persistence of CTC at 3 to 4 weeks after the treatment was started and at the time of restaging continued to be significantly associated with prognosis, particularly in women with hormone receptor-negative disease and women who were receiving chemotherapy.
Epigenetic changes, such as DNA methylation, are one of the most common molecular alterations in human neoplasia (Egger et al, 2004), including breast cancer (Widschwendter and Jones, 2002). DNA methylation refers to the addition of a methyl group to the cytosine ring of those cytosines that precede a guanosine (referred to as CpG dinucleotides) to form 5-methylcytosine. CpG dinucleotides are found at increased frequency in the promoter region of many genes, and methylation in the promoter regions is frequently associated with gene silencing (Leonhardt and Cardoso, 2000). Several studies have shown that tumour-specific epigenetic alterations can be detected in DNA recovered from plasma or serum of patients with various malignancies (Wong et al, 1999; Silva et al, 1999a; Sanchez-Cespedes et al, 2000), a finding that may be of particular clinical interest in view of molecular diagnosis and prognosis. Increased concentrations of free DNA are detected in the blood of many cancer patients, whereas only small amounts of free circulating DNA are found in healthy individuals (Leon et al, 1977). The serum of breast cancer patients contains, on an average, approximately four times more free DNA compared with that of healthy individuals (Gal et al, 2004). Recently, investigators have shown that hypermethylation of ras association domain family protein 1A (RASSF1A) and/or adenomatous polyposis coli (APC) identified in serum DNA from breast cancer patients is associated with a worse outcome (Müller et al, 2003). Furthermore, methylated RASSF1A and neurogenic differentiation 1 gene promoters in serum are candidate biomarkers for monitoring the efficacy of adjuvant therapy in breast cancer patients (Fiegl et al, 2005, 2008).
The precise mechanism by which DNA is released into the bloodstream still remains enigmatic. The most common hypothesis advanced for circulating DNA in the blood of cancer patients is that it is because of the lysis of CTC (Stroun et al, 2000). Other possible sources include DNA leakage from cells as the result of tumour necrosis or apoptosis, or spontaneous release of DNA into the circulation from primary and metastatic tumours (Stroun et al, 2000). Although many studies have suggested the usefulness of CTC or cell-free DNA as a surrogate marker of subclinical metastasis for breast cancer (Taback et al, 2001; Huang et al, 2006; Ntoulia et al, 2006; Wong et al, 2006; Wülfing et al, 2006; Xenidis et al, 2006; Quintela-Fandino et al, 2006), few studies have looked into the relation between CTC and cell-free DNA in this type of cancer (Schwarzenbach et al, 2004). A combined molecular assessment of the circulating DNA and CTC could improve the evaluation of cancer stage and overall prognosis in breast cancer.
The aim of this study was to identify tumour-specific epigenetic alterations in the cell-free DNA found in the peripheral blood of breast cancer patients and to assess whether a correlation exists between total or tumour-specific methylated DNA and the detection of CTC in peripheral blood of patients with metastatic breast cancer. We decided to investigate these molecular markers in women with metastatic disease because CTC and the circulating DNA levels are known to be higher in these patients.
Materials and methods
Patients and sample collection
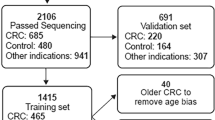
We prospectively obtained matched peripheral blood, serum and plasma samples from 80 patients with breast cancer and 20 healthy volunteers. All patients gave informed consent for the use of their blood specimen and the examination of blood samples was carried out after approval from the Institutional Review Board of the General Hospital Sint-Augustinus (Wilrijk, Belgium). The patient population consisted of four patients with localised breast cancer (group A), 60 patients with metastatic breast cancer receiving treatment (group B) and 16 patients presenting in our clinic with untreated metastatic breast cancer (group C). Clinicopathological variables are listed in Table 1. The median age of the control population was 39 (range, 25–54) years and 62 (range, 34–85) years in the breast cancer population.
Blood samples from patients with metastatic disease were taken during the course of treatment. Disease status was assessed using the RECIST (Response Evaluation Criteria in Solid Tumours Group) criteria without the knowledge of the patients' CTC or circulating DNA results (Therasse et al, 2000). Stable disease was measured up to 8 weeks after the initiation of therapy.
In 18 cases, the corresponding breast cancer tissue samples were available for analysis. All tumour tissues were obtained immediately after surgical resection and snap frozen in liquid nitrogen.
Quantitative analysis of total DNA
Blood (4.5 ml) from each donor was collected in 0.129 M sodium citrate-containing tubes (Becton Dickinson, Franklin Lakes, NJ, USA) and centrifuged (2000g, 10 min) at room temperature. Then, plasma was aliquotted and cryopreserved at −80°C until use. DNA was extracted from 200 μl of plasma using the JETQUICK Blood and Cell Culture Kit (Genomed, Löhne, Germany) according to the manufacturer's protocol, with an elution volume of 100 μl. Plasma DNA concentration was measured by a real-time quantitative PCR assay for the human telomerase reverse transcriptase gene using the Quantifiler Human DNA Quantification Kit (Applied Biosystems, Foster City, CA, USA). The assay included two primers and a FAM-labelled fluorescent TaqMan probe for the target gene, and two primers and a VIC-labelled fluorescent TaqMan probe for an internal control DNA sequence. For construction of the calibration curve, we generated a standard curve using three-fold serial dilutions of known concentrations of DNA (50, 16.67, 5.56, 1.85, 0.62, 0.21 and 0.023 ng μl–1). PCR was carried out in a final reaction volume of 25 μl and contained 12.5 μl of Quantifiler PCR Reaction Mix (Applied Biosystems), 10.5 μl of Quantifiler Human Primer Mix (Applied Biosystems) and 2 μl of extracted DNA. Each sample was analysed in duplicate.
The mean quantity of each duplicate calculated by the 7900 sequence detection system software was used for further analysis. The concentration, expressed in nanograms per millilitre, was calculated using the following equation: C=Q × VDNA/VPCR × 1/Vext × 1000, where C=target concentration in plasma (nanograms per millilitre); Q=target quantity (nanograms); VDNA=total volume of extraction (100 μl); VPCR=volume of DNA solution used per PCR reaction (2 μl); and Vext=volume of plasma extracted (200 μl).
Methylated DNA assay
Blood (8 ml) from each donor was collected in serum separator tubes (Becton Dickinson) and centrifuged (2000g, 10 min) at room temperature. Then, serum was aliquotted and cryopreserved at −80°C until use. Genomic DNA was extracted from 1 ml of serum using the ZR Serum DNA Kit (Zymo Research, Orange, CA, USA), with an elution volume of 35 μl. Genomic DNA from frozen breast cancer tissues was isolated using the QIAamp DNA Mini Kit (Qiagen, Valencia, CA, USA). Sodium bisulphite conversion of extracted DNA was conducted using the EZ DNA Methylation Kit (Zymo Research). Sodium bisulphite-converted DNA was analysed by real-time qMSP. Two sets of primers and probes, designed specifically for sodium bisulphite-converted DNA, were used: a methylated set for the genes of interest and a reference set, β-actin (ACTB), to normalise for input DNA. Fluorogenic probes and PCR primer sets for APC (Usadel et al, 2002), RASSF1A (Lehmann et al, 2002), oestrogen receptor 1 (ESR1) (Eads et al, 2001) and ACTB (Eads et al, 2000) were custom synthesised by Applied Biosystems. Fluorogenic PCRs were carried out in a reaction volume of 25 μl in 96-well plates in a 7900HT Sequence Detector (Applied Biosystems). PCR was carried out in separate wells for each primer/probe set, and each sample was run in duplicate. The final reaction mixture consisted of 600 nmol l–1 of each primer, 200 nmol l–1 of probe and 12.5 μl of Universal Master Mix (Applied Biosystems). Five μl of the treated DNA solution was used in each real-time MSP reaction. Thermal cycling was initiated with a first denaturation step of 95°C for 10 min. The thermal profile for the PCR was 95°C for 15 s and 60°C for 1 min. Data obtained during 50 cycles of amplification were analysed. Each plate included water blanks, a positive control and a negative control. DNA isolated from normal peripheral lymphocytes from healthy individuals served as a negative methylation control. In vitro methylated human DNA (Zymo Research) was used as the positive methylation control.
The ratio between the values obtained in the two TaqMan analyses was used as a measure for the degree of methylation of the target gene. The percentage of fully methylated molecules at a gene locus was calculated by dividing the gene : ACTB ratio of a sample by the gene : ACTB ratio of fully methylated human DNA and multiplying by 100. We use the abbreviation percentage of methylated reference (PMR) to indicate this measurement. A gene was deemed methylated if the PMR value was >0.
CTC assay
Peripheral blood (10 ml) was collected from each donor into CellSave blood collection tubes (Immunicon Inc., Huntingdon Valley, PA, USA), which are evacuated blood-draw tubes containing EDTA and a cellular preservative, and processed within a maximum of 72 h after blood drawing (at room temperature).
Circulating tumour cells were enumerated with the CellSearch System (Veridex, Warren, NJ, USA) as described by Allard et al (2004). Briefly, 7.5 ml of blood were gently mixed with 6.5 ml of dilution buffer, centrifuged (800 × g, 10 min, gentle deceleration) at room temperature and transferred into the CellTracks AutoPrep system (Veridex, Warren, NJ, USA). After aspiration of the plasma and dilution buffer layer, anti-EpCAM antibody-coated ferrofluids were added. After incubation and magnetic separation, unbound cells and remaining plasma were removed, and ferrofluid-labelled cells were re-suspended in buffer, permeabilised, and fluorescently labelled using phycoerythrin-conjugated anti-cytokeratin antibodies recognising cytokeratins (predominantly cytokeratins 8, 18 and 19) to specifically identify epithelial cells, an antibody against CD45 conjugated with allophycocyanin to identify WBC and a nuclear dye (4′,6-diamidino-2-phenylindole (DAPI)) to fluorescently label the cell nuclei. The sample was transferred automatically to a cartridge in a MagNest (Veridex, Warren, NJ, USA), where the immunomagnetically labelled cells move to the surface caused by the strong magnetic field of the MagNest device. The MagNest was placed on the CellTracks Analyzer II (Veridex, Warren, NJ, USA), a four-color semi-automated fluorescence microscope, and image frames covering the entire surface of the cartridge for each of the four fluorescent filter cubes were captured. The captured images containing objects that met predetermined criteria were automatically presented in a web-enabled browser from which final selection of cells was made by the operator. The main criteria for an object to be defined as a CTC included round to oval morphology, a visible nucleus (DAPI positive), positive staining for cytokeratin and negative staining for CD45. Results of cell enumeration were expressed as the number of cells per 7.5 ml of blood, and a cutoff of ⩾2 CTC was chosen to define the test as positive. Each sample was analysed independently by two readers (HJ Elst and PB Vermeulen). Questionable interpretations were evaluated again until consensus was reached.
Statistical analysis
We used Pearson's χ2 or, in the case of low frequencies per cell, Fisher's exact method to test associations between categorical variables. The Mann–Whitney U-test or the Kruskal–Wallis test was used to assess the differences between non-parametric distributed variables. A two-sided P⩽0.05 was considered to be statistically significant. All statistical calculations were carried out using SPSS, version 11.0 (SPSS Inc, Chicago, IL, USA).
Results
Total DNA concentrations in plasma from healthy volunteers and breast cancer patients
The median concentration of plasma DNA in the healthy controls (n=20) was 4 ng ml–1 (range 0–17 ng ml–1). The median value for breast cancer patients (n=80) was 13 ng ml–1 (range 2–2027 ng ml–1). The median values and ranges for the different groups of breast cancer patients were as follows: 7 (4–12) ng ml–1 for group A (n=4), 12 (2–123) ng ml–1 for group B (n=60) and 29 (4–2027) ng ml–1 for group C (n=16) (Figure 1). The difference between the patients and the controls was statistically significant (P<0.001). Differences between plasma DNA concentrations in different patients groups also reached statistical significance (P=0.04). The largest differences were measurable between groups A and C (P=0.02) and groups B and C (P=0.06).
The plasma DNA levels were significantly correlated with CA15.3 levels (r=0.276, P=0.02) and tended to be correlated with tumour progression, although this was not statistically significant: median total DNA levels were 11 (range, 3–94) ng ml–1 in patients with stable disease (n=27) and 20 (range, 2–2027) ng ml–1 in patients with progressive disease (n=46) (P=0.09). Plasma DNA concentrations were positively associated with patient age (r=0.298, P=0.007). No associations with ER, PR, HER2 and p53 were found.
Receiver-operating characteristics (ROC) curve analysis was carried out to define cutoff DNA levels for the prediction of malignancy (Figure 2). The area under the ROC curve assessing plasma DNA concentration was 0.865 (95% confidence interval, 0.782–0.948), suggesting a good discriminative power of the molecular assay. Table 2 lists several cut-off points of DNA values used for the generation of the ROC curve with their sensitivity and specificity. The highest accuracy was obtained at the cut-off point of 8.275 ng ml–1 with a sensitivity of 72.5% and a specificity of 85%. We divided patients into high plasma DNA level group (HDNA) and low plasma DNA level group (LDNA) according to the cut-off value identified in the ROC curve analysis. Overall, 85% of patients with progressive disease were in the HDNA group, whereas there were only 59% with stable disease in the HDNA group (P=0.01) (Table 3a). Again, no associations were found with ER, PR, HER2 and p53.
Receiver-operating characteristics curve for plasma total DNA concentration in 20 healthy individuals and 80 patients with breast cancer, plotting the true positive rate (sensitivity) against the false positive rate (1-specificity) for the different possible cut-off points. The area under the curve was 0.865, suggesting a good discriminative power of the molecular assay.
Detection of tumour-related methylated DNA in serum
We selected a panel of three genes, namely, APC, RASSF1A and ESR1, for the detection of tumour-specific methylated DNA in serum samples from healthy controls (n=19) and breast cancer patients (n=79). Median PMR values of APC and RASSF1A, but not of ESR1, were significantly higher among breast cancer cases as compared with controls (P<0.05). Methylation of APC was positively associated with the methylation of RASSF1A (r=0.372, P=0.001), but not with methylation of ESR1 (Figure 3). The distribution of PMR in the patient and control groups is shown for all three genes in Figure 4. PMR values of APC (r=0.398, P=0.001), RASSF1A (r=0.551, P<0.001), but not of ESR1 (r=0.078, P=0.52), were positively correlated with levels of the tumour marker CA15.3. No associations were found between PMR values of the three genes and age of the patient.
Correlations between methylation levels for the three genes. A significant correlation was observed between percentage of methylated reference (PMR) values for adenomatous polyposis coli (APC) and ras association domain family protein 1A (RASSF1A) (C) and between PMR values for RASSF1A and oestrogen receptor 1 (ESR1) (B). No clear correlation was observed between PMR values for APC and ESR1 (A).
Methylation levels of (A) adenomatous polyposis coli (APC), (B) ras association domain family protein 1A (RASSF1A) and (C) oestrogen receptor 1 (ESR1) in serum DNA of healthy controls (n=19) and breast cancer patients (n=79). Differences in percentage of methylated reference (PMR) values between patients and controls were examined with the Mann–Whitney U-test. For APC and RASSF1A significantly higher PMR values were observed in patients versus controls (P=0.04 and P=0.003, respectively). For ESR1, differences in PMR values between patients and controls did not reach statistical significance (P=0.33).
Detection of any level of aberrant methylation (PMR>0) resulted in a specificity for detecting breast cancer of 95% for APC, 100% for RASSF1A and 89.5% for ESR1. The frequency of methylation in serum DNA of APC and RASSF1A was significantly higher among women with breast cancer as compared with controls: APC, 29 versus 5% (P=0.03) and RASSF1A, 35 versus 0% (P=0.002). However, the association of methylation in serum DNA of ESR1 with case status did not reach statistical significance: ESR1 was hypermethylated in 20% of breast cancer patients and 10.5% of healthy controls (P=0.33). Of the 79 patients with breast cancer, 7 (9%) had all the three methylated markers, 18 (23%) had at least two methylated markers and 42 (53%) had at least one methylated marker in serum. Of all two-marker combinations, the combination of APC and/or RASSF1A methylation was most frequently observed, in 47% of breast cancer cases. Methylation of multiple genes in serum DNA was not detected in any of the 19 controls. The difference in the number of methylated genes between breast cancer patients and controls was statistically significant (P=0.003).
The detection of at least one methylated marker in serum was associated with the disease status (P=0.02) (Table 3b). Hypermethylation of both APC and RASSF1A, but not of ESR1, was more frequently detected in patients with progressive disease as compared with patients with stable disease (P=0.08 and P=0.001, respectively). Hypermethylation of RASSF1A was significantly associated with ER expression (P=0.01) and HR status (P=0.007), which was defined as positive if ER and/or PR were positive (Table 2). No associations were found with PR status, HER2 status, triple negative (ER–, PR– and HER2–) tumours and p53 status. No significant associations were found between hypermethylation of ESR1 and APC and any of the clinicopathological variables (Table 1). Although there were no statistically significant differences in detection of aberrant methylation by age among breast cancer patients, each gene was more likely to be aberrantly methylated in older (>60y) compared with younger participants with breast cancer (Table 4).
In 18 cases, the corresponding breast cancer tissue samples were available for analysis. ESR1 was methylated in all tissue samples, whereas APC was unmethylated in one case and RASSF1A in three cases. All of the genes found to be methylated in serum samples were also methylated in the corresponding tissue sample. Comparison of PMR values of breast cancer tissue samples between unmethylated and methylated serum samples for each investigated gene showed no significant results (Figure 5). Median PMR values in, respectively, unmethylated and methylated serum samples were 72 (range, 0–143) and 125 (range, 1–361) for APC (P=0.21), 12 (range, 0–63) and 48 (range, 1–67) for RASSF1A (P=0.127) and 1.2 (range, 0.2–3.5) and 1.3 (range, 0.7–3.7) for ESR1 (P=0.64).
Comparison of percentage of methylated reference (PMR) values in breast cancer tissue between unmethylated (negative) and methylated (positive) serum samples for (A) adenomatous polyposis coli (APC), (B) ras association domain family protein 1A (RASSF1A) and (C) oestrogen receptor 1 (ESR1). Differences in PMR values between unmethylated and methylated serum samples were examined with the Mann–Whitney U-test. For none of the genes did these differences reach statistical significance.
Detection of CTC in peripheral blood
Overall, positive cells were identified in the blood of 65% of breast cancer patients and 10% of controls (Figure 6). Numbers of CTC were significantly higher in blood samples of patients with breast cancer than in healthy controls: the median number of CTC detected in 7.5 ml of blood was 1 (range, 0–2617) in breast cancer patients and 0 (range 0–1) in controls (P<0.001). Numbers of CTC also tended to differ between different patients groups, although this was not statistically significant: no CTC were detected in group A, the median number of CTC in group B was 1 (0–2617) and the median number of CTC in group C was 0.5 (0–153) (P=0.07). CTC numbers by the CellSearch System were significantly correlated with the patients' age (r=0.380, P=0.001) and CA15.3 levels (r=0.685, P<0.001). Furthermore, the number of CTC tended to be higher in ER+ breast tumours (P=0.09) and HER2– breast tumours (P=0.08), although this was not statistically significant.
Using ⩾2 cells as a threshold for positive samples in the patient population, which corresponded to 100% specificity in the control population, 34% of samples from patients were positive with the CellSearch System. A significant association was observed between CTC and tumour progression: in 22 of 46 (48%) patients with progressive disease CTC were detected, whereas only in 5 of 26 (9%) patients with stable disease CTC were present (P=0.02) (Table 3c).
Association between CTC and total plasma DNA or serum methylated DNA
The concentration of total DNA in plasma was significantly correlated with the number of CTC detected in peripheral blood (r=0.368, P=0.001) (Figure 7). Patients with CTC in peripheral blood had significantly higher plasma total DNA levels than patients with no CTC: median DNA concentrations were, respectively, 10 (range, 2–118) ng ml–1 and 31 (3–2027) ng ml–1 (P=0.002) (Table 5a). PMR values for APC (r=0.314, P=0.005) and RASSF1A (r=0.492, P<0.001) were significantly correlated with the number of CTC detected in peripheral blood. No associations were found between PMR values for ESR1 and CTC. In patients with at least one gene methylated in serum (n=42), CTC were detected in 19 (45%) cases. In patients without any methylation in serum DNA (n=36), no CTC were detected in 28 (78%) cases. Detection of a methylated gene in serum was significantly associated with the detection of CTC in peripheral blood (P=0.03) (Table 5b). Also the number of methylated genes in serum was significantly correlated with the presence of CTC in paired specimens (P=0.01).
CTC, total and/or methylated DNA as predictive markers of tumour progression
Next, we evaluated the correlation of the three molecular markers (high plasma total DNA, presence of CTC and methylated markers in serum) with tumour progression. Overall, 18% of breast cancer patients were positive for all the three molecular markers (high plasma DNA, at least one methylated gene in serum and ⩾2 CTC), 56% of breast cancer patients were positive for at least two molecular markers, 82% of breast cancer patients were positive for at least one molecular marker and 18% of breast cancer patients were negative for all three markers. Of 19 healthy controls, 13 (68%) were negative for all three markers. The presence of multiple markers was not detected in the control population.
Of all patients with stable disease (n=25), two (8%) were positive for all three markers, nine (36%) were positive for ⩾2 markers, 19 (76%) were positive for at least one marker and six (24%) were completely negative. In contrast, of all patients with progressive disease (n=46), 16 (35%) were positive for all the three markers, 34 (74%) were positive for ⩾2 markers, 42 (91%) were positive for at least one marker and four (9%) were completely negative (P=0.01) (Table 3d).
Discussion
Circulating DNA is present in plasma in healthy controls and is increased in cancer patients (Leon et al, 1977). These findings have attracted much attention to the potential use of elevated concentrations of circulating total DNA as a tumour marker. In this study, we measured the level of circulating DNA in the plasma of healthy controls and patients with localised or metastatic breast cancer using a real-time quantitative PCR method. Our results show a 3.25-fold difference in the median levels of circulating total DNA in plasma between breast cancer patients and healthy controls. The ROC curve result shows a good association between high DNA concentration and malignancy. The range of total DNA levels in the circulation of breast cancer patients varied widely, from levels like those in the controls (2–17 ng ml–1) to levels that exceeded values of 2000 ng ml–1 plasma. The highest values were measured in patients presenting in our clinic with untreated metastatic disease. Furthermore, total DNA levels tended to correlate with the tumour serum marker CA15.3, which is a high molecular glycoprotein (mucin) that can be detected in the peripheral blood of breast cancer patients. Although in patients with primary breast cancer the concentration of CA15.3 is usually within the normal range, increased levels of CA15.3 are often observed in patients with metastatic disease and correlate with an increased metastatic load (Antoine et al, 1994).
Circulating nucleic acids harbouring tumour-specific alterations have been identified in serum or plasma from breast cancer patients (Silva et al, 1999a). Methylated DNA markers are attractive tumour markers in blood for several reasons: (a) DNA in blood is stable, is easy to obtain and can be analysed by a high-throughput method such as qMSP; (b) methylated DNA markers are frequently found in a wide range of human cancers and not (or rarely) in healthy controls (Silva et al, 1999a, 1999b; Wong et al, 1999; Goessl et al, 2000; Sanchez-Cespedes et al, 2000; (c) in general, a high concordance between epigenetic alterations in primary tumour specimens and in blood has been reported (Usadel et al, 2002; Hoque et al, 2004; Topaloglu et al, 2004; Yang et al, 2004); (d) they are not limited to patients with metastatic cancer, but are also present in body fluid from patients with early or organ-confined tumours (Esteller et al, 1999; Sanchez-Cespedes et al, 2000). As no single gene is known to be hypermethylated in more than a proportion of breast tumours, it is necessary to use a panel of genes to provide a target for detection in serum. We selected three genes, namely, APC, RASSF1A and ESR1, which are known to be frequently hypermethylated in breast cancer (Widschwendter and Jones, 2002). We decided to measure methylation levels of these genes in serum instead of plasma, as Müller et al (2003) indicated the prognostic relevance of methylated DNA coding for these three genes in pre-therapeutic serum samples of patients with primary breast cancer (Müller et al 2003). Furthermore, to date, their remains no consensus as to whether plasma or serum is better for the assessment of circulating methylated DNA in cancer patients' blood. Overall, 53% of breast cancer patients showed hypermethylation of at least one of the three genes. RASSF1A had the highest frequency of hypermethylation with 35% of breast cancer cases being positive, followed by APC and ESR1 being methylated in 29 and 20% of breast cancer cases, respectively. Methylation in serum DNA was never detected if this alteration was not present in the primary tumour tissue. We found no correlation between methylated DNA levels in serum and corresponding levels in the primary tumour tissue. This could be because of the specific physiological characteristics in the progression of each tumour, for example, angiogenic capacity, the ability to cause local necrosis (Usadel et al, 2002; Widschwendter et al, 2004a). Alternatively, the quantity and quality of DNA templates extracted from serum or the original primary tumour can differ on the basis of time of collection, the content of DNAse and other factors (Usadel et al, 2002; Widschwendter et al, 2004a) or the presence of normal DNA in blood may obscure minute amounts of circulating tumour-related DNA.
Methylation was also detected in a small proportion of controls (16%). Methylation of several genes has been reported earlier in non-malignant tissues and serum DNA of smokers. Detection of methylation in serum DNA could be a marker of disease (an early neoplastic effect), exposure (a biological effect of any environmental factor) or both (Hoque et al, 2006).
Our most interesting finding of correlating methylation data to clinicopathological variables was the strong association between methylation of RASSF1A in serum DNA and HR status. Methylation of RASSF1A in breast cancer has already been connected to hormone regulation, but the mechanism is not clear yet. Widschwendter et al. reported significant differences in the HR status between clusters of DNA methylation profiles (Widschwendter et al, 2004b). Feng et al. investigated whether methylation of a set of growth-suppressor genes would correlate with the expression of ER and PR, and found that methylation of RASSF1A was strongly correlated with ER, PR and HR expression (Feng et al, 2007). Also in the study by Sunami et al., hypermethylation of RASSF1A was more frequently present in ER+ breast tumours than in ER– breast tumours (Sunami et al, 2008). Thus, it seems that epigenetic alterations in the RASSF1A gene promoter and HR regulation in breast cancer are tightly linked.
Using the CellSearch System, at least one positive cell was identified in the blood of 65% of breast cancer patients and 10% of controls. It has been reported that false positive results using immuno-mediated CTC detection techniques can occur by specific labelling of non-tumour epithelial cells or non-specific labelling of non-tumour non-epithelial cells (Paterlini-Brechot and Benali, 2007). Variable numbers of epithelial cells have been found in peripheral blood of subjects without malignancy, being related to benign epithelial proliferative diseases, inflammation, tissue trauma, semi-surgical and surgical interventions (Crisan et al, 2000; Goeminne et al, 2000; Fehm et al, 2005).
To date, there is no agreement on the mechanisms that are responsible for the presence of tumour DNA shed into the bloodstream. The most common hypothesis is the shedding of lysed CTC. However, this seems to be unlikely because the number of CTC is inadequate to explain the observed amount of DNA in the plasma or serum (Stroun et al, 2000). Other possibilities are that apoptosis and necrosis of tumour cells increase the levels of circulating DNA (Jahr et al, 2001) or that DNA is actively released into the bloodstream by the tumour (Stroun et al, 2000). In this study, we observed a good association between total DNA or tumour-specific DNA levels and the number of CTC in blood from breast cancer patients. Patients with CTC in peripheral blood had significantly higher plasma total DNA levels than patients with no CTC. PMR values for APC and RASSF1A were significantly correlated with the number of CTC detected in peripheral blood. Furthermore, a combination assessment of these three molecular markers could predict tumour progression. Similar findings to ours have been reported earlier in patients with melanoma (Koyanagi et al, 2006). Koyanagi et al. showed that the detection of CTC was correlated with tumour-related methylated DNA and that a combined assessment of both molecular markers improved the assessment of prognosis in stage IV melanoma patients treated with biochemotherapy. However, Schwarzenbach et al. did not observe a correlation between the incidence of loss of heterozygosity in circulating DNA and the presence of CTC in the blood from breast cancer patients (Schwarzenbach et al, 2004). The observed correlation between CTC and circulating methylated DNA in our study could be interpreted in two ways: (a) CTC are a potential source of circulating tumour-specific DNA; (b) high numbers of CTC and circulating methylated DNA are both a phenotypic feature of more aggressive tumour biology.
In conclusion, this study provides evidence that the detection of large amounts of free circulating total DNA and of methylated genes are associated with CTC in peripheral blood from patients with advanced breast cancer. Furthermore, the combined assessment of all three molecular markers was predictive for tumour progression. However, large-scale studies are necessary to verify the clinical utility of CTC and serum methylated DNA as potential prognostic factors in breast cancer patients.
Change history
16 November 2011
This paper was modified 12 months after initial publication to switch to Creative Commons licence terms, as noted at publication
References
Allard WJ, Matera J, Miller M, Repollet M, Connelly M, Rao C, Tibbe A, Uhr JW, Terstappen L (2004) Tumour cells circulate in the peripheral blood of all major carcinomas but not in healthy subjects or patients with nonmalignant diseases. Clin Cancer Res 10: 6897–6904
Antoine E, Kayitalire L, Spielmann M (1994) CA 15-3 and breast cancer. Rev Med Interne 15: 650–662
Benoy I, Elst H, Philips M, Wuyts H, Van Dam P, Scharpe S, Van Marck E, Vermeulen P, Dirix L (2006) Prognostic significance of disseminated tumour cells as detected by quantitative real-time reverse-transcriptase polymerase chain reaction in patients with breast cancer. Clin Breast Cancer 7: 146–152
Braun S, Vogl F, Naume B, Janni W, Osborne M, Coombes R, Schlimok G, Diel I, Gerber B, Gebauer G, Pierga J, Marth C, Oruzio D, Wiedswang G, Solomayer E, Kundt G, Strobl B, Fehm T, Wong G, Bliss J, Vincent-Salomon A, Pantel K (2005) A pooled analysis of bone marrow micrometastasis in breast cancer. N Engl J Med 353: 793–802
Crisan D, Ruark DS, Decker DA, Drevon AM, Dicarlo RG (2000) Detection of circulating epithelial cells after surgery for benign breast disease. Mol Diagn 5: 33–38
Cristofanilli M, Budd GT, Ellis MJ, Stopeck A, Matera J, Miller MC, Reuben JM, Doyle GV, Allard WJ, Terstappen LW, Hayes DF (2004) Circulating tumor cells, disease progression, and survival in metastatic breast cancer. N Engl J Med 351: 781–791
Cristofanilli M, Hayes DF, Budd GT, Ellis MJ, Stopeck A, Reuben JM, Doyle GV, Matera J, Allard WJ, Miller MC, Fritsche HA, Hortobagyi GN, Terstappen LW (2005) Circulating tumor cells: a novel prognostic factor for newly diagnosed metastatic breast cancer. J Clin Oncol 23: 1420–1430
Eads C, Lord R, Wickramasinghe K, Long T, Kurumboor S, Bernstein L, Peters J, Demeester S, Demeester T, Skinner K, Laird P (2001) Epigenetic patterns in the progression of esophageal adenocarcinoma. Cancer Res 61: 3410–3418
Eads CA, Danenberg KD, Kawakami K, Saltz LB, Blake C, Shibata D, Danenberg PV, Laird PW (2000) MethyLight: a high-throughput assay to measure DNA methylation. Nucl Acids Res 28: e32
Egger G, Liang G, Aparicio A, Jones PA (2004) Epigenetics in human disease and prospects for epigenetic therapy. Nature 429: 457–463
Esteller M, Sanchez-Cespedes M, Rosell R, Sidransky D, Baylin SB, Herman JG (1999) Detection of aberrant promoter hypermethylation of tumour suppressor genes in serum DNA from non-small cell lung cancer patients. Cancer Res 59: 67–70
Fehm T, Solomayer EF, Meng S, Tucker T, Lane N, Wang J, Gebauer G (2005) Methods for isolating circulating epithelial cells and criteria for their classification as carcinoma cells. Cytotherapy 7: 171–185
Feng W, Shen L, Wen S, Rosen DG, Jelinek J, Hu X, Huan S, Huang M, Liu J, Sahin AA, Hunt KK, Bast RC, Shen Y, Issa JP, Yu Y (2007) Correlation between CpG methylation profiles and hormone receptor status in breast cancers. Breast Cancer Res 9: R57
Fiegl H, Jones A, Hauser-Kronberger C, Hutarew G, Reitsamer R, Jones RL, Dowsett M, Mueller-Holzner E, Windbichler G, Daxenbichler G, Goebel G, Ensinger C, Jacobs I, Widschwendter M (2008) Methylated NEUROD1 promoter is a marker for chemosensitivity in breast cancer. Clin Cancer Res 14: 3494–3502
Fiegl H, Millinger S, Mueller-Holzner E, Marth C, Ensinger C, Berger A, Klocker H, Goebel G, Widschwendter M (2005) Circulating tumour-specific DNA: a marker for monitoring efficacy of adjuvant therapy in cancer patients. Cancer Res 65: 1141–1145
Gal S, Fidler C, Lo YM, Taylor M, Han C, Moore J, Harris AL, Wainscoat JS (2004) Quantitation of circulating DNA in the serum of breast cancer patients by real-time PCR. Br J Cancer 90: 1211–1215
Goeminne JC, Guillaume T, Symann M (2000) Pitfalls in the detection of disseminated non-hematological tumor cells. Ann Oncol 11: 785–792
Goessl C, Krause H, Müller M, Heicappell R, Schrader M, Sachsinger J, Miller K (2000) Fluorescent methylation-specific polymerase chain reaction for DNA-based detection of prostate cancer in bodily fluids. Cancer Res 60: 5941–5945
Hoque MO, Begum S, Topaloglu O, Jeronimo C, Mambo E, Westra WH, Califano JA, Sidransky D (2004) Quantitative detection of promoter hypermethylation of multiple genes in the tumour, urine, and serum DNA of patients with renal cancer. Cancer Res 64: 5511–5517
Hoque MO, Feng Q, Toure P, Dem A, Critchlow CW, Hawes SE, Wood T, Jeronimo C, Rosenbaum E, Stern J, Yu M, Trink B, Kiviat NB, Sidransky D (2006) Detection of aberrant methylation of four genes in plasma DNA for the detection of breast cancer. J Clin Oncol 24: 4262–4269
Huang ZH, Li LH, Hua D (2006) Quantitative analysis of plasma circulating DNA at diagnosis and during follow-up of breast cancer patients. Cancer Lett 243: 64–70
Jahr S, Hentze H, Englisch S, Hardt D, Fackelmayer FO, Hesch RD, Knippers R (2001) DNA fragments in the blood plasma of cancer patients: quantitations and evidence for their origin from apoptotic and necrotic cells. Cancer Res 61: 1659–1665
Koyanagi K, Mori T, O′day SJ, Martinez SR, Wang HJ, Hoon DS (2006) Association of circulating tumour cells with serum tumour-related methylated DNA in peripheral blood of melanoma patients. Cancer Res 66: 6111–6117
Lehmann U, Langer F, Feist H, Glockner S, Hasemeier B, Kreipe H (2002) Quantitative assessment of promoter hypermethylation during breast cancer development. Am J Pathol 160: 605–612
Leon S, Shapiro B, Sklaroff D, Yaros M (1977) Free DNA in the serum of cancer patients and the effect of therapy. Cancer Res 37: 646–650
Leonhardt H, Cardoso MC (2000) DNA methylation, nuclear structure, gene expression and cancer. J Cell Biochem Suppl 35 (Suppl): 78–83
Muller HM, Widschwendter A, Fiegl H, Ivarsson L, Goebel G, Perkmann E, Marth C, Widschwendter M (2003) DNA methylation in serum of breast cancer patients: an independent prognostic marker. Cancer Res 63: 7641–7645
Ntoulia M, Stathopoulou A, Ignatiadis M, Malamos N, Mavroudis D, Georgoulias V, Lianidou ES (2006) Detection of Mammaglobin A-mRNA-positive circulating tumor cells in peripheral blood of patients with operable breast cancer with nested RT-PCR. Clin Biochem 39: 879–887
Pantel K, Cote RJ, Fodstad O (1999) Detection and clinical importance of micrometastatic disease. J Natl Cancer Inst 91: 1113–1124
Paterlini-Brechot P, Benali NL (2007) Circulating tumor cells (CTC) detection: clinical impact and future directions. Cancer Lett 253: 180–204
Quintela-Fandino M, Lopez JM, Hitt R, Gamarra S, Jimeno A, Ayala R, Hornedo J, Guzman C, Gilsanz F, Cortes-Funes H (2006) Breast cancer-specific mRNA transcripts presence in peripheral blood after adjuvant chemotherapy predicts poor survival among high-risk breast cancer patients treated with high-dose chemotherapy with peripheral blood stem cell support. J Clin Oncol 24: 3611–3618
Sanchez-Cespedes M, Esteller M, Wu L, Nawroz-Danish H, Yoo GH, Koch WM, Jen J, Herman JG, Sidransky D (2000) Gene promoter hypermethylation in tumours and serum of head and neck cancer patients. Cancer Res 60: 892–895
Schwarzenbach H, Müller V, Stahmann N, Pantel K (2004) Detection and characterization of circulating microsatellite-DNA in blood of patients with breast cancer. Ann NY Acad Sci 1022: 25–32
Silva JM, Dominguez G, Garcia JM, Gonzalez R, Villanueva MJ, Navarro F, Provencio M, San M (1999a) Presence of tumour DNA in plasma of breast cancer patients: clinicopathological correlations. Cancer Res 59: 3251–3256
Silva JM, Dominguez G, Villanueva MJ, Gonzalez R, Garcia JM, Corbacho C, Provencio M, España P, Bonilla F (1999b) Aberrant DNA methylation of the p16INK4a gene in plasma DNA of breast cancer patients. Br J Cancer 80: 1262–1264
Stroun M, Maurice P, Vasioukhin V, Lyautey J, Lederrey C, Lefort F, Rossier A, Chen XQ, Anker P (2000) The origin and mechanism of circulating DNA. Ann NY Acad Sci 906: 161–168
Sunami E, Shinozaki M, Sim MS, Nguyen SL, Vu AT, Giuliano AE, Hoon DS (2008) Estrogen receptor and HER2/neu status affect epigenetic differences of tumour-related genes in primary breast tumours. Breast Cancer Res 10: R46
Taback B, Giuliano AE, Hansen NM, Hoon DS (2001) Microsatellite alterations detected in the serum of early stage breast cancer patients. Ann NY Acad Sci 945: 22–30
Therasse P, Arbuck SG, Eisenhauer EA, Wanders J, Kaplan RS, Rubinstein L, Verweij J, Van Glabbeke M, van Oosterom AT, Christian MC, Gwyther SG (2000) New guidelines to evaluate the response to treatment in solid tumors. European Organization for Research and Treatment of Cancer, National Cancer Institute of the United States, National Cancer Institute of Canada. J Natl Cancer Inst 92: 205–216
Topaloglu O, Hoque MO, Tokumaru Y, Lee J, Ratovitski E, Sidransky D, Moon CS (2004) Detection of promoter hypermethylation of multiple genes in the tumour and bronchoalveolar lavage of patients with lung cancer. Clin Cancer Res 10: 2284–2288
Usadel H, Brabender J, Danenberg KD, Jeronimo C, Harden S, Engles J, Danenberg PV, Yang S, Sidransky D (2002) Quantitative adenomatous polyposis coli promoter methylation analysis in tumour tissue, serum, and plasma DNA of patients with lung cancer. Cancer Res 62: 371–375
Widschwendter A, Muller H, Fiegl H, Ivarsson L, Wiedemair A, Muller-Holzner E, Goebel G, Marth C, Widschwendter M (2004a) DNA methylation in serum and tumours of cervical cancer patients. Clin Cancer Res 10: 565–571
Widschwendter M, Jones PA (2002) DNA methylation and breast carcinogenesis. Oncogene 21: 5462–5482
Widschwendter M, Siegmund KD, Muller HM, Fiegl H, Marth C, Muller-Holzner E, Jones PA, Laird PW (2004b) Association of breast cancer DNA methylation profiles with hormone receptor status and response to tamoxifen. Cancer Res 64: 3807–3813
Wong IH, Lo YM, Zhang J, Liew CT, Ng MH, Wong N, Lai PB, Lau WY, Hjelm NM, Johnson PJ (1999) Detection of aberrant p16 methylation in the plasma and serum of liver cancer patients. Cancer Res 59: 71–73
Wong NS, Kahn HJ, Zhang L, Oldfield S, Yang LY, Marks A, Trudeau ME (2006) Prognostic significance of circulating tumour cells enumerated after filtration enrichment in early and metastatic breast cancer patients. Breast Cancer Res Treat 99: 63–69
Wülfing P, Borchard J, Buerger H, Heidl S, Zänker KS, Kiesel L, Brandt B (2006) HER2-positive circulating tumor cells indicate poor clinical outcome in stage I to III breast cancer patients. Clin Cancer Res 12: 1715–1720
Xenidis N, Perraki M, Kafousi M, Apostolaki S, Bolonaki I, Stathopoulou A, Kalbakis K, Androulakis N, Kouroussis C, Pallis T, Christophylakis C, Argyraki K, Lianidou ES, Stathopoulos S, Georgoulias V, Mavroudis D (2006) Predictive and prognostic value of peripheral blood cytokeratin-19 mRNA-positive cells detected by real-time polymerase chain reaction in node-negative breast cancer patients. J Clin Oncol 24: 3756–3762
Yang HJ, Liu VW, Wang Y, Chan KY, Tsang PC, Khoo US, Cheung AN, Ngan HY (2004) Detection of hypermethylated genes in tumour and plasma of cervical cancer patients. Gynecol Oncol 93: 435–440
Acknowledgements
Ilse Van der Auwera is a research assistant of the Fund for Scientific Research Flanders. Furthermore, we would like to thank the Clinical Trial Organisation from the General Hospital Sint-Augustinus for their assistance.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
From twelve months after its original publication, this work is licensed under the Creative Commons Attribution-NonCommercial-Share Alike 3.0 Unported License. To view a copy of this license, visit http://creativecommons.org/licenses/by-nc-sa/3.0/
About this article
Cite this article
Van der Auwera, I., Elst, H., Van Laere, S. et al. The presence of circulating total DNA and methylated genes is associated with circulating tumour cells in blood from breast cancer patients. Br J Cancer 100, 1277–1286 (2009). https://doi.org/10.1038/sj.bjc.6605013
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.bjc.6605013
Keywords
This article is cited by
-
Overexpression of Stat3 increases circulating cfDNA in breast cancer
Breast Cancer Research and Treatment (2021)
-
Detection and monitoring of hypermethylated RASSF1A in serum from patients with metastatic breast cancer
Clinical Epigenetics (2016)
-
Circulating DNA as biomarker in breast cancer
Breast Cancer Research (2015)
-
Silver Nanoscale Hexagonal Column Chips for Detecting Cell-free DNA and Circulating Nucleosomes in Cancer Patients
Scientific Reports (2015)
-
Role of Circulating Cell-Free DNA in Cancers
Molecular Diagnosis & Therapy (2015)