Abstract
In the last few years, V-domain Ig-containing suppressor of T cell activation(VISTA) has been reported as a prognostic biomarker in articles including various solid tumours. However, their conclusions have been controversial. For this reason, we performed this meta-analysis to further verify the prognostic value of VISTA in solid tumours. All relevant literature was identified from PubMed, Embase, the Cochrane Library and Web of Science. Ten studies, including 2, 440 patients, were eligible for the analysis. The pooled results showed that high expression of VISTA was associated with favourable overall survival (OS) than that seen with low expression of VISTA (7 studies, hazard ratio (HR) = 0.75, 95% confidence interval (CI): 0.66–0.86, P < 0.001). In addition, high expression of VISTA significantly correlated with high numbers of CD8 (+) tumour infiltrating lymphocytes (TILs) (3 studies, risk ratio (RR) = 1.80, 95% CI: 1.41–2.31, P < 0.001). In conclusion, these results indicate that VISTA is a potential prognostic biomarker in solid tumours.
Similar content being viewed by others
Introduction
V-domain Ig-containing suppressor of T cell activation (VISTA), also known as PD-1H, is a member of the immunoglobulin (Ig) superfamily, whose extracellular domain bears homology to the B7 family ligand programmed death ligand 1 (PD-L1). In both mice1 and humans2, VISTA is predominantly expressed on granulocytic, myeloid cells and T cells. Similar to some members of the B7-CD28 family3, T cells both express and respond to VISTA4. In vitro proliferation assays, VISTA suppressed the proliferation of both CD4 (+) and CD8 (+) T cells. In mouse tumour models of methylcholanthrene 105-induced fibrosarcoma, Wang1 found that overexpression of VISTA on tumour cells accelerated tumour growth. More recently, Le Mercier5 reported that a VISTA monoclonal antibody synergized with a tumour vaccine to impair the growth of established B16-BL6 tumours. These studies suggest that VISTA is a novel negative checkpoint regulator.
Recently, a number of studies have reported the expression of VISTA in the tumour microenvironment of human solid tumours, and these studies found that VISTA was a potential prognostic biomarker associated with patients’ survival. However, their conclusions were controversial. Villarroel6 found that high levels of VISTA correlated with better overall survival (OS) in non-small-cell lung cancer (NSCLC) than low levels of VISTA. Loeser’s study7 showed the same trend in esophageal adenocarcinoma (EAC). In contrast, Kuklinski’s study8 showed that high expression of VISTA was associated with poor disease-specific survival (DSS). Therefore, further research is needed to better illustrate the prognostic value of VISTA.
In this study, a systematic review of the eligible literature on this topic was performed by us using the PubMed, Embase, the Cochrane Library and Web of Science databases. Then, a meta-analysis of the survival rates (including OS, DSS and tumour-specific survival (TSS)) of patients expressing different levels of VISTA was conducted. Our results indicated that high expression of VISTA, compared with low expression of VISTA, correlated with better OS and high numbers of CD8 (+) tumour infiltrating lymphocytes (TILs).
Results
Characteristics of the included studies
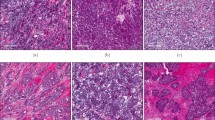
As presented in Fig. 1, a total of 8 articles6,7,8,9,10,11,12,13, including 10 studies and 2,440 patients, met the inclusion criteria for the meta-analysis. The main characteristics of the included studies are shown in Table 1. The publish year of all included articles was between 2017 and 2019. The Newcastle–Ottawa Scale14 (NOS; Supplementary Table 1) was used to assess the included studies. Approximately one-third of the studies were conducted in Asia (n = 3). The remaining studies were conducted in North America (n = 4) and Europe (n = 3). Cancer types included hepatocellular carcinoma (HCC), oral squamous cell carcinoma(OSCC), NSCLC, ovarian cancer (OC), primary cutaneous melanoma(PCM), gastric cancer(GC), EAC and malignant pleural mesothelioma(MPM). The sample size of the included studies ranged from 65 to 464. The expression level of VISTA in included studies is presented in Supplementary Table 2. Among the 10 studies, 7 studies explored the prognostic value of VISTA in terms of patients’ OS, 2 studies explored the TSS, and 1 study explored the DSS. As far as we understand, the data regarding TSS and DSS can be combined into one group.
Methodological quality of the included studies
The quality of the included studies was generally high. All of the studies had an independent assessment of outcome. The majority of the included studies had long enough follow-up durations (5 years), and most of them provided an adequate follow-up. However, none of these eligible studies had representativeness of the exposed cohort because the study objects were patients selected from the hospital. In the majority of the studies, methods for handling intention-to-treat analysis and missing data were not described adequately.
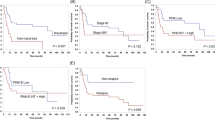
High expression of VISTA in solid tumours is associated with favourable OS
Seven studies6,7,11,12,13 reported the relationship between the expression of VISTA and patients’ OS. We applied a fixed effect model to calculate the pooled hazard ratio (HR) and 95% confidence interval (CI) because there was no obvious heterogeneity (P = 0.564, I2 = 0.0%). The results showed that high expression of VISTA was associated with better OS than low expression of VISTA. (HR = 0.75, 95% CI: 0.66–0.86, P < 0.001, Fig. 2a).
The prognostic value of VISTA in patients’ DSS(or TSS)
Three studies8,9,10 reported the relationship between the expression of VISTA and patients’ DSS (or TSS). A random effect model was applied to calculate the pooled HR and 95% CI due to obvious heterogeneity (P = 0.003, I2 = 82.6%). However, no obvious trend in DSS (or TSS) was found according to the expression of VISTA (HR = 1.57, 95% CI: 0.71–3.48, P = 0.268, Fig. 2b).
High expression of VISTA correlates with high numbers of CD8 (+) TILs
To further analyse the possible factors that may affect the prognostic value of VISTA in solid tumours, we researched the correlation between the expression of VISTA and patients’ clinicopathological characteristics. Interestingly, we found that high expression of VISTA was significantly associated with high numbers of CD8 (+) TILs (risk ratio (RR) = 1.80, 95% CI: 1.41–2.31, P < 0.001, Fig. 3). As shown in Table 2, no obvious trend in TNM stage or gender was found according to the expression of VISTA.
Sensitivity analysis and publication bias
Studies with high NOS scores (≥7) were included in the sensitivity analysis of the association between the expression of VISTA and patients’ OS. As shown in Fig. 4, there was no change in the trend regarding HR and 95% CI. High expression of VISTA correlated with a better OS than low expression of VISTA in the high NOS scores studies. According to the guideline, publication bias should not be assessed when the included studies are less than 10, so we did not evaluate the publication bias.
Discussion
As far as we know, this is the first study to systematically evaluate the prognostic value of VISTA in human solid tumours. Our results revealed that high expression of VISTA was associated with better OS. To further analyse the possible factors that may affect the prognostic value of VISTA in solid tumours, we investigated the correlation between the expression of VISTA and patients’ clinicopathological characteristics. The results indicated that high expression of VISTA significantly correlated with high numbers of CD8 ( + ) TILs.
In the last few years, a number of molecules, such as PD-L1, programmed death 1(PD-1), lymphocyte activation gene 3(LAG3) and T cell immunoglobulin- and mucin-domain-containing molecule-3(TIM3) have been considered as negative immune checkpoints. In 2014, Lines2 first defined VISTA as a new negative immune checkpoint. In vitro proliferation assays, VISTA suppressed the proliferation of both CD4+ and CD8+ T cells. In mouse models, VISTA blockade decelerated tumour growth, and overexpression of VISTA accelerated tumour growth. As described above, it seemed that VISTA was associated with poor prognosis. However, Villarroel6 found that high levels of VISTA correlated with better OS in NSCLC. Coincidentally, Loeser’s study6 showed the same trend in esophageal adenocarcinoma. Moreover, we found the same trends not only in the studies of VISTA, but also in some studies of other negative immune molecules, such as PD-1 and PD-L115,16,17,18,19,20. Badoua showed that PD-1+ TILs were associated with favourable OS in human papillomavirus(+) head and neck cancer. Similarly, Zhu’s study demonstrated that high expression of PD-L1 on tumour cells correlated with better OS than that seen in nasopharyngeal carcinoma patients with low expression of PD-L1. The reasons that may account for this discrepancy include biological differences between mice and humans, different types of tumours and the subjective evaluation of immunohistochemistry (IHC) or immunofluorescence (IF) scores.
Recently, an increasing number of researchers21,22,23,24,25,26,27,28,29 have paid great attention to the CD8 (+) TILs in the tumour microenvironment due to their anti-tumour effect. Gabrielson’s research21 illustrated that high numbers of CD8 (+) TILs significantly correlated with a low rate of recurrence and prolonged relapse-free survival in patients with HCC. Goode22 showed that in high-grade serous ovarian cancer, high numbers of CD8 (+) TILs were significantly associated with improved OS. Ye28 found that high numbers of CD8 (+) TILs predicted favourable prognosis in lung adenocarcinoma patients. These studies may indicate that CD8 (+) TILs are a prognostic biomarker that correlates with a favourable prognosis in solid tumours. In our study, we found that high expression of VISTA was remarkably associated with high numbers of CD8 (+) TILs. This result may partly account for the conclusion that high expression of VISTA correlates with favourable OS in solid tumours.
In conclusion, VISTA may act as a positive prognostic biomarker in solid tumours. Nevertheless, due to the current rarity of studies of the association between the expression of VISTA and patients’ prognosis in solid tumours, we cannot assess publication bias. Therefore, more studies are required for further analysis.
Methods
Literature search strategy
We searched all relevant literature in Embase, PubMed, the Cochrane Library and Web of Science on September 28th, 2019, without language restriction. These databases were thoroughly searched by the following strategy: ((((((((((VISTA[Title/Abstract] OR VSIR[Title/Abstract]) OR B7H5[Title/Abstract]) OR GI24[Title/Abstract]) OR B7-H5[Title/Abstract]) OR Dies1[Title/Abstract]) OR PD-1H[Title/Abstract]) OR SISP1[Title/Abstract]) OR PP2135[Title/Abstract]) OR C10orf54[Title/Abstract])OR DD1alpha[Title/Abstract]) AND (((cancer[Title/Abstract] OR tumor[Title/Abstract]) OR tumour[Title/Abstract]) OR carcinoma[Title/Abstract]). Two investigators (X.L.H. and Y.Z) independently checked all eligible articles. They reached an agreement via mutual discussion to solve any discrepancies.
Inclusion criteria
Studies eligible for inclusion met the following rules:(1) the studies detected the expression of VISTA in human solid tumor by IHC or IF; (2) the association of the expression of VISTA and OS/DSS/TSS in solid tumours was reported; (3) HR and 95% CI were reported or could be extracted in the articles or supplementary materials; (4) articles were published as research papers.
Exclusion criteria
The exclusion criteria included the following: (1) the articles were conference abstracts or reviews; (2) full text of the article was not available; (3) the studies used animal models.
Data extraction and quality assessment
Information was independently extracted by two researchers (H.Z.L. and Q.X.L.) from the included studies. The collected information included the name of first author, publication year, study country, cancer type, sample size, gender, detection method of the expression of VISTA, cut-off value, TNM stage, and outcome including OS and DSS(or TSS). Two investigators (H.Z.L. and Q.X.L.) independently estimated the HRs and 95% CIs of survival data via Cox univariate analysis. When the articles only provided Kaplan-Meier curves, Engauge Digitizer 4.1 and spreadsheets provided by Tierney30 and Parmar31 were used to estimate the HRs and 95% CIs. When there were discrepancies, another investigator (X.L.H.) participated in the process. Two investigators(H.Z.L. and Q.X.L.) evaluated the included studies’ quality independently by the NOS(scores: 0–9), and we defined studies that had high NOS scores (≥7) as high-quality. The investigators reached an agreement by mutual discussing when there were inconsistent results.
Statistical analysis
The association between the expression of VISTA and patients’ prognosis was evaluated by meta-analysis by collecting data from all included studies. We calculated outcome endpoints including OS, DSS and TSS via pooled HRs and 95% CIs. HRs > 1 indicated a poor prognosis. The correlation between the expression of VISTA and the clinicopathological characteristics was evaluated by pooled RRs and 95% CIs. Cochrane’s Q statistic and the I2 statistic were used to assess the heterogeneity among the included studies. A random effects model was used to calculate pooled HRs and 95% CIs when there was substantial heterogeneity (Q test: P < 0.1 or an I2 > 50%). If not, a fixed effects model was used. Studies of high quality(NOS scores ≥ 7) were selected for sensitivity analysis. RevMan 5.3 and Stata 12.0 statistical software (Stata Corporation, College Station, TX, USA) were used to perform all statistical analyses. A difference was considered significant with a two-tailed p < 0.05.
References
Wang, L. et al. VISTA, a novel mouse Ig superfamily ligand that negatively regulates T cell responses. Journal of Experimental Medicine 208, 577–592, https://doi.org/10.1084/jem.20100619 (2011).
Lines, J. L. et al. VISTA is an immune checkpoint molecule for human T cells. Cancer research 74, 1924–1932, https://doi.org/10.1158/0008-5472.CAN-13-1504 (2014).
Butte, M. J., Keir, M. E., Phamduy, T. B., Sharpe, A. H. & Freeman, G. J. Programmed death-1 ligand 1 interacts specifically with the B7-1 costimulatory molecule to inhibit T cell responses. Immunity 27, 111–122, https://doi.org/10.1016/j.immuni.2007.05.016 (2007).
Lines, J. L., Sempere, L. F., Broughton, T., Wang, L. & Noelle, R. VISTA is a novel broad-spectrum negative checkpoint regulator for cancer immunotherapy. Cancer immunology research 2, 510–517, https://doi.org/10.1158/2326-6066.CIR-14-0072 (2014).
Le Mercier, I. et al. VISTA regulates the development of protective antitumor immunity. Cancer research 74, 1933–1944, https://doi.org/10.1158/0008-5472.CAN-13-1506 (2014).
Villarroel-Espindola, F. et al. Spatially Resolved and Quantitative Analysis of VISTA/PD-1H as a Novel Immunotherapy Target in Human Non-Small Cell Lung Cancer. Clinical cancer research: an official journal of the American Association for Cancer Research 24, 1562–1573, https://doi.org/10.1158/1078-0432.ccr-17-2542 (2018).
Loeser, H. et al. The expression of the immune checkpoint regulator VISTA correlates with improved overall survival in pT1/2 tumor stages in esophageal adenocarcinoma. Oncoimmunology 8, e1581546, https://doi.org/10.1080/2162402x.2019.1581546 (2019).
Kuklinski, L. F. et al. VISTA expression on tumor-infiltrating inflammatory cells in primary cutaneous melanoma correlates with poor disease-specific survival. Cancer Immunology, Immunotherapy 67, 1113–1121, https://doi.org/10.1007/s00262-018-2169-1 (2018).
Böger, C., Behrens, H. M., Krüger, S. & Röcken, C. The novel negative checkpoint regulator VISTA is expressed in gastric carcinoma and associated with PD-L1/PD-1: A future perspective for a combined gastric cancer therapy? Oncoimmunology 6, https://doi.org/10.1080/2162402X.2017.1293215 (2017).
Liao, H., Zhu, H., Liu, S. & Wang, H. Expression of V-domain immunoglobulin suppressor of t cell activation is associated with the advanced stage and presence of lymph node metastasis in ovarian cancer. Oncology letters 16, 3465–3472, https://doi.org/10.3892/ol.2018.9059 (2018).
Wu, L. et al. Expression of VISTA correlated with immunosuppression and synergized with CD8 to predict survival in human oral squamous cell carcinoma. Cancer Immunology, Immunotherapy 66, 627–636, https://doi.org/10.1007/s00262-017-1968-0 (2017).
Zhang, M. et al. VISTA expression associated with CD8 confers a favorable immune microenvironment and better overall survival in hepatocellular carcinoma. BMC cancer 18, https://doi.org/10.1186/s12885-018-4435-1 (2018).
Muller, S. et al. V-domain Ig-containing suppressor of T-cell activation (VISTA), a potentially targetable immune checkpoint molecule, is highly expressed in epithelioid malignant pleural mesothelioma. Modern pathology: an official journal of the United States and Canadian Academy of Pathology, Inc, https://doi.org/10.1038/s41379-019-0364-z (2019).
Wells, G., Shea, B. & O’Connell, J. The Newcastle-Ottawa Scale (NOS) for Assessing The Quality of Nonrandomised Studies in Meta-analyses, 7, http://www.ohri.ca/programs/clinical_epidemiology/oxford.asp (2014).
Badoual, C. et al. PD-1-expressing tumor-infiltrating T cells are a favorable prognostic biomarker in HPV-associated head and neck cancer. Cancer research 73, 128–138, https://doi.org/10.1158/0008-5472.can-12-2606 (2013).
De Meulenaere, A. et al. Tumor PD-L1 status and CD8(+) tumor-infiltrating T cells: markers of improved prognosis in oropharyngeal cancer. Oncotarget 8, 80443–80452, https://doi.org/10.18632/oncotarget.19045 (2017).
Hanna, G. J. et al. Tumor PD-L1 expression is associated with improved survival and lower recurrence risk in young women with oral cavity squamous cell carcinoma. International journal of oral and maxillofacial surgery 47, 568–577, https://doi.org/10.1016/j.ijom.2017.09.006 (2018).
Kogashiwa, Y. et al. PD-L1 Expression Confers Better Prognosis in Locally Advanced Oral Squamous Cell Carcinoma. Anticancer research 37, 1417–1424, https://doi.org/10.21873/anticanres.11465 (2017).
Vassilakopoulou, M. et al. Evaluation of PD-L1 Expression and Associated Tumor-Infiltrating Lymphocytes in Laryngeal Squamous Cell Carcinoma. Clinical cancer research: an official journal of the American Association for Cancer Research 22, 704–713, https://doi.org/10.1158/1078-0432.ccr-15-1543 (2016).
Zhu, Q. et al. Tumor cells PD-L1 expression as a favorable prognosis factor in nasopharyngeal carcinoma patients with pre-existing intratumor-infiltrating lymphocytes. Oncoimmunology 6, e1312240, https://doi.org/10.1080/2162402x.2017.1312240 (2017).
Gabrielson, A. et al. Intratumoral CD3 and CD8 T-cell Densities Associated with Relapse-Free Survival in HCC. Cancer immunology research 4, 419–430, https://doi.org/10.1158/2326-6066.cir-15-0110 (2016).
Goode, E. L. et al. Dose-Response Association of CD8+ Tumor-Infiltrating Lymphocytes and Survival Time in High-Grade Serous Ovarian Cancer. JAMA oncology 3, e173290, https://doi.org/10.1001/jamaoncol.2017.3290 (2017).
Hoesli, R. et al. Proportion of CD4 and CD8 tumor infiltrating lymphocytes predicts survival in persistent/recurrent laryngeal squamous cell carcinoma. Oral oncology 77, 83–89, https://doi.org/10.1016/j.oraloncology.2017.12.003 (2018).
Li, J., Wang, J., Chen, R., Bai, Y. & Lu, X. The prognostic value of tumor-infiltrating T lymphocytes in ovarian cancer. Oncotarget 8, 15621–15631, https://doi.org/10.18632/oncotarget.14919 (2017).
Liang, Y., Lu, W., Zhang, X. & Lu, B. Tumor-infiltrating CD8+ and FOXP3+ lymphocytes before and after neoadjuvant chemotherapy in cervical cancer. Diagnostic pathology 13, 93, https://doi.org/10.1186/s13000-018-0770-4 (2018).
Nguyen, N. et al. Tumor infiltrating lymphocytes and survival in patients with head and neck squamous cell carcinoma. Head & neck 38, 1074–1084, https://doi.org/10.1002/hed.24406 (2016).
Rashed, H. E., Abdelrahman, A. E., Abdelgawad, M., Balata, S. & Shabrawy, M. E. Prognostic Significance of Programmed Cell Death Ligand 1 (PD-L1), CD8+ Tumor-Infiltrating Lymphocytes and p53 in Non-Small Cell Lung Cancer: An Immunohistochemical Study. Turk patoloji dergisi 1, 211–222, https://doi.org/10.5146/tjpath.2017.01398 (2017).
Ye, S. L., Li, X. Y., Zhao, K. & Feng, T. High expression of CD8 predicts favorable prognosis in patients with lung adenocarcinoma: A cohort study. Medicine 96, e6472, https://doi.org/10.1097/md.0000000000006472 (2017).
Zhou, C. et al. Density and location of CD3(+) and CD8(+) tumor-infiltrating lymphocytes correlate with prognosis of oral squamous cell carcinoma. Journal of oral pathology & medicine: official publication of the International Association of Oral Pathologists and the American Academy of Oral Pathology 47, 359–367, https://doi.org/10.1111/jop.12698 (2018).
Tierney, J. F., Stewart, L. A., Ghersi, D., Burdett, S. & Sydes, M. R. Practical methods for incorporating summary time-to-event data into meta-analysis. Trials 8, 16, https://doi.org/10.1186/1745-6215-8-16 (2007).
Parmar, M. K., Torri, V. & Stewart, L. Extracting summary statistics to perform meta-analyses of the published literature for survival endpoints. Statistics in medicine 17, 2815–2834 (1998).
Author information
Authors and Affiliations
Contributions
X.L.H. and Y.Z. conceived and made the decision of this topic, analyzed the data and wrote the paper. Z.W. reviewed drafts of the paper and participated in its design. Q.X.L. and H.Z.L. evaluated the included studies’ quality by NOS scores and extracted the data. The final manuscript has been read and approved by all the authors.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
He, XL., Zhou, Y., Lu, HZ. et al. Prognostic value of VISTA in solid tumours: a systematic review and meta-analysis. Sci Rep 10, 2662 (2020). https://doi.org/10.1038/s41598-020-59608-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-020-59608-w
This article is cited by
-
Superpixel image segmentation of VISTA expression in colorectal cancer and its relationship to the tumoral microenvironment
Scientific Reports (2021)
-
Prognostic significance and therapeutic potential of the immune checkpoint VISTA in pancreatic cancer
Journal of Cancer Research and Clinical Oncology (2021)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.