Abstract
Ductal carcinoma in situ (DCIS) represents the earliest identifiable breast cancer lesion. Disruption of the myoepithelial cell layer and basement membrane is a prerequisite for DCIS to initiate invasion into the stroma. The majority of epithelial cells overlying a focally-disrupted myoepithelial cell layer are estrogen receptor-alpha negative (ER(−)); however, adjacent cells within the same duct confined by an intact myoepithelial cell layer express high levels of ER. These ER (+) and ER (−) cells were microdissected from the same ducts of breast cancer patients. Differential proteins expressed by ER(+) and ER(−) cells were identified using two-dimensional gel electrophoresis followed by mass spectrometry and Western blot analysis. ER(−) cells express lower levels of superoxide dismutase, RalA binding protein, galectin-1, uridine phosphorylase 2, cellular retinoic acid-binding protein 1, S100 calcium binding protein A11, and nucleoside diphosphate kinase A or non-metastasis protein 23-H1 (nm23-H1). The upregulated protein, Rho GDP-dissociation inhibitor 1 alpha, may induce chemotherapy resistance. The significant findings are that the microdissected ER(−) cells express 12.6 times less cellular retinoic acid-binding protein 1, a protein involved in cellular differentiation, and 4.1 times less nucleoside diphosphate kinase A or nm23-H1, a metastasis suppressor, and express fewer proteins than adjacent ER(+) cells. The collective role of the alterations of protein expression in ER(−) cells may be to promote a more malignant phenotype than adjacent ER(+) cells, including a decreased ability to undergo apoptosis and differentiation, and an increased potential to damage DNA, metastasize, and resist to chemotherapy.




Similar content being viewed by others
Abbreviations
- CRABP1:
-
Cellular retinoic acid-binding protein 1
- DCIS:
-
Ductal carcinoma in situ
- 2-DE:
-
Two-dimensional gel electrophoresis
- DTT:
-
Dithiothreitol
- ERα:
-
Estrogen receptor alpha
- IPG:
-
Immobilized pH gradient
- MALDI-TOF-MS:
-
Matrix-assisted laser desorption-ionization time-of-flight mass spectrometry
- ME cells:
-
Myoepithelial cells
- M r :
-
Molecular mass
- NDPK-A (or nm23-H1):
-
Nucleoside diphosphate kinase A (non-metastasis protein 23-H1)
- OG:
-
Octylglucopyranoside
- pI:
-
Isoelectric point
- RhoGDIα:
-
Rho GDP-dissociation inhibitor 1 alpha
- S100A11:
-
S100 calcium binding protein A11
- UPase:
-
Uridine phosphorylase
- SMA:
-
Smooth muscle actin
References
Skinner KA, Silverstein MJ (2001) The management of ductal carcinoma in situ of the breast. Endocr Relat Cancer 8(1):33–45
Jones JL (2006) Overdiagnosis and overtreatment of breast cancer: progression of ductal carcinoma in situ: the pathological perspective. Breast Cancer Res 8(2):204
Jolicoeur F, Seemayer TA, Gabbiani G et al (2002) Multifocal, nascent, and invasive myoepithelial carcinoma (Malignant myoepithelioma) of the breast: an immunohistochemical and ultrastructural study. Int J Surg Path 10(4):281–291
Nerlich AG, Haraida S, Hagedorn H et al (1995) Morphological aspects of basement-membranes and their receptors in benign and malignant neoplasms. Int J Oncol 6(6):1193–1202
Tsubura A, Shikata N, Inui T et al (1988) Immunohistochemical localization of myoepithelial cells and basement-membrane in normal, benign and malignant human-breast lesions. Virchows Archiv A Pathol Anat Histopathol 413(2):133–139
Man YG, Sang QXA (2004) The significance of focal myoepithelial cell layer disruptions in human breast tumor invasion: a paradigm shift from the “protease-centered” hypothesis. Exp Cell Res 301(2):103–118
Gustafsson JA (1999) Estrogen receptor beta—a new dimension in estrogen mechanism of action. J Endocrinol 163(3):379–383
Green S, Walter P, Kumar V et al (1986) Human estrogen-receptor cDNA—sequence, expression and homology to V-Erb-A. Nature 320(6058):134–139
Greene GL, Gilna P, Waterfield M et al (1986) Sequence and expression of human estrogen-receptor complementary-DNA. Science 231(4742):1150–1154
Kuiper G, Enmark E, Pelto-Huikko M et al (1996) Cloning of a novel estrogen receptor expressed in rat prostate and ovary. Proc Natl Acad Sci USA 93(12):5925–5930
Mosselman S, Polman J, Dijkema R (1996) ER beta: identification and characterization of a novel human estrogen receptor. FEBS Lett 392(1):49–53
Anderson E, Clarke R, Laidlaw I et al (1996) Experiments on proliferation of normal human breast tissue in nude mice do not show that progesterone does not stimulate breast cells: reply. Endocrinology 137(4):1505–1506
Skliris GP, Munot K, Bell SM et al (2003) Reduced expression of oestrogen receptor beta in invasive breast cancer and its re-expression using DNA methyl transferase inhibitors in a cell line model. J Pathol 201(2):213–220
Bardin A, Boulle N, Lazennec G et al (2004) Loss of ER beta expression as a common step in estrogen-dependent tumor progression. Endocr Relat Cancer 11(3):537–551
Park BW, Kim KS, Heo MK et al (2003) Expression of estrogen receptor-beta in normal mammary and tumor tissues: is it protective in breast carcinogenesis? Breast Cancer Res Treat 80(1):79–85
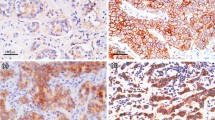
Man YG, Tai L, Barner R et al (2003) Cell clusters overlying focally disrupted mammary myoepithelial cell layers and adjacent cells within the same duct display different immunohistochemical and genetic features: implications for tumor progression and invasion. Breast Cancer Res 5(6):R231–R241
Man YG, Shekitka KM, Bratthauer GL et al (2002) Immunohistochemical and genetic alterations in mammary epithelial cells immediately overlying focally disrupted myoepithelial cell layers. Breast Cancer Res Treat 76:S143–S143
Yousefi M, Mattu R, Gao CL et al (2005) Mammary ducts with and without focal myoepithelial cell layer disruptions show a different frequency of white blood cell infiltration and growth pattern: Implications for tumor progression and invasion. Appl Immunohistochem Mol Morphol 13(1):30–37
Sauter ER, Zhu W, Fan XJ et al (2002) Proteomic analysis of nipple aspirate fluid to detect biologic markers of breast cancer. Br J Cancer 86(9):1440–1443
Li JN, Zhang Z, Rosenzweig J et al (2002) Proteomics and bioinformatics approaches for identification of serum biomarkers to detect breast cancer. Clin Chem 48(8):1296–1304
Sahab ZJ, Semaan SM, Sang QXA (2007) Methodology and applications of disease biomarker identification in human serum. Biomark Insights 2:21–43
O’Neill KA, Miller FR, Barder TJ et al (2003) Profiling the progression of cancer: separation of microsomal proteins in MCF10 breast epithelial cell lines using nonporous chromatophoresis. Proteomics 3(7):1256–1269
Wu WG, Tang XM, Hu W et al (2002) Identification and validation of metastasis-associated proteins in head and neck cancer cell lines by two-dimensional electrophoresis and mass spectrometry. Clin Exp Metastasis 19(4):319–326
Ornstein DK, Gillespie JW, Paweletz CP et al (2000) Proteomic analysis of laser capture microdissected human prostate cancer and in vitro prostate cell lines. Electrophoresis 21(11):2235–2242
Wulfkuhle JD, Sgroi DC, Krutzsch H et al (2002) Proteomics of human breast ductal carcinoma in situ. Cancer Res 62(22):6740–6749
Bischoff R, Luider TM (2004) Methodological advances in the discovery of protein and peptide disease markers. J Chromatogr B Analyt Technol Biomed Life Sci 803(1):27–40
Somiari RI, Sullivan A, Russell S et al (2003) High-throughput proteomic analysis of human infiltrating ductal carcinoma of the breast. Proteomics 3(10):1863–1873
Hanash SM (2000) Biomedical applications of two-dimensional electrophoresis using immobilized pH gradients: current status. Electrophoresis 21(6):1202–1209
Sahab ZJ, Suh Y, Sang QXA (2005) Isoelectric point-based prefractionation of proteins from crude biological samples prior to two-dimensional gel electrophoresis. J Proteome Res 4(6):2266–2272
Binz PA, Hochstrasser DF, Appel RD (2003) Mass spectrometry-based proteomics: current status and potential use in clinical chemistry. Clin Chem Lab Med 41(12):1540–1551
Aebersold R, Mann M (2003) Mass spectrometry-based proteomics. Nature 422(6928):198–207
Ferguson PL, Smith RD (2003) Proteome analysis by mass spectrometry. Annu Rev Biophys Biomol Struct 32:399–424
Heck AJR, Krijgsveld J (2004) Mass spectrometry-based quantitative proteomics. Expert Rev Proteomics 1(3):317–326
Feuerstein I, Rainer M, Bernardo K et al (2005) Derivatized cellulose combined with MALDI-TOF MS: a new tool for serum protein profiling. J Proteome Res 4(6):2320–2326
Sahab ZJ, Iczkowski KA, Sang QXA (2007) Anion exchange fractionation of serum proteins versus albumin elimination. Anal Biochem 368(1):24–32
Karas M, Hillenkamp F (1988) Laser desorption ionization of proteins with molecular masses exceeding 10000 Daltons. Anal Chem 60(20):2299–2301
Tanaka K, Waki H, Ido Y et al (1988) Protein and polymer analyses up to m/z 100,000 by laser ionization time-of-flight mass spectrometry. Rapid Commun Mass Spectrom 2(8):151–153
Schiller J, Arnhold J, Benard S et al (1999) Lipid analysis by matrix-assisted laser desorption and ionization mass spectrometry: a methodological approach. Anal Biochem 267(1):46–56
Briehl MM, Baker AF, Siemankowski LM et al (1997) Modulation of antioxidant defenses during apoptosis. Oncol Res 9(6–7):281–285
Oberley LW, Buettner GR (1979) Role of superoxide-dismutase in cancer—review. Cancer Res 39(4):1141–1149
Tchevkina E, Agapova L, Dyakova N et al (2005) The small G-protein RalA stimulates metastasis of transformed cells. Oncogene 24(3):329–335
Ward Y, Wang W, Woodhouse E et al (2001) Signal pathways which promote invasion and metastasis: critical and distinct contributions of extracellular signal-regulated kinase and Ral-specific guanine exchange factor pathways. Mol Cell Biol 21(17):5958–5969
Jullien-Flores V, Dorseuil O, Romero F et al (1995) Bridging Ral GTPase to Rho pathways. RLIP76, a Ral effector with CDC42/Rac GTPase-activating protein activity. J Biol Chem 270(38):22473–22477
Lim KH, O’Hayer K, Adam SJ et al (2006) Divergent roles for RalA and RalB in malignant growth of human pancreatic carcinoma cells. Curr Biol 16(24):2385–2394
Park SH, Weinberg RA (1995) A putative effector of Ral has homology to Rho/Rac GTPase activating proteins. Oncogene 11(11):2349–2355
Nobes CD, Hall A (1995) Rho, rac, and cdc42 GTPases regulate the assembly of multimolecular focal complexes associated with actin stress fibers, lamellipodia, and filopodia. Cell 81(1):53–62
Awasthi S, Cheng J, Singhal SS (2000) Novel function of human RLIP76: ATP-dependent transport of glutathione conjugates and doxorubicin. Biochemistry 39(31):9327–9334
Sasaki T, Takai Y (1998) The Rho small G protein family Rho GDI system as a temporal and spatial determinant for cytoskeletal control. Biochem Biophys Res Commun 245(3):641–645
Olofsson B (1999) Rho guanine dissociation inhibitors: pivotal molecules in cellular signalling. Cell Signal 11(8):545–554
Fritz G, Brachetti C, Bahlmann F et al (2002) Rho GTPases in human breast tumours: expression and mutation analyses and correlation with clinical parameters. Br J Cancer 87(6):635–644
Zhang BL, Zhang YQ, Dagher MC et al (2005) Rho GDP dissociation inhibitor protects cancer cells against drug-induced apoptosis. Cancer Res 65(14):6054–6062
Wells V, Davies D, Mallucci L (1999) Cell cycle arrest and induction of apoptosis by beta galactoside binding protein (beta GBP) in human mammary cancer cells. A potential new approach to cancer control. Eur J Cancer 35(6):978–983
Rabinovich GA (2005) Galectin-1 as a potential cancer target. Br J Cancer 92(7):1188–1192
Jung EJ, Moon HG, Cho BI et al (2007) Galectin-1 expression in cancer-associated stromal cells correlates tumor invasiveness and tumor progression in breast cancer. Int J Cancer 120(11):2331–2338
Cao DL, Russell RL, Zhang DK et al (2002) Uridine phosphorylase (−/−) murine embryonic stem cells clarify the key role of this enzyme in the regulation of the pyrimidine salvage pathway and in the activation of fluoropyrimidines. Cancer Res 62(8):2313–2317
Yan R, Wan LX, Pizzorno G et al (2006) Uridine phosphorylase in breast cancer: a new prognostic factor? Front Biosci 11:2759–2766
Kawamura K, Takiguchi N, Wada A et al (2006) Up-regulated expression of the uridine phosphorylase gene in human gastric tumors is correlated with a favorable prognosis. Anticancer Res 26(6C):4647–4651
Gorry P, Lufkin T, Dierich A et al (1994) The cellular retinoic acid-binding protein-I is dispensable. Proc Natl Acad Sci USA 91(19):9032–9036
Dong D, Ruuska SE, Levinthal DJ et al (1999) Distinct roles for cellular retinoic acid-binding proteins I and II in regulating signaling by retinoic acid. J Biol Chem 274(34):23695–23698
Kondo A, Sakaguchi M, Makino E et al (2002) Localization of S100C immunoreactivity in various human tissues. Acta Med Okayama 56(1):31–34
Oue N, Hamai Y, Mitani Y et al (2004) Gene expression profile of gastric carcinoma: identification of genes and tags potentially involved in invasion, metastasis, and carcinogenesis by serial analysis of gene expression. Cancer Res 64(7):2397–2405
Memon AA, Sorensen BS, Meldgaard P et al (2005) Down-regulation of S100C is associated with bladder cancer progression and poor survival. Clin Cancer Res 11(2):606–611
Steeg PS, Bevilacqua G, Kopper L et al (1988) Evidence for a novel gene associated with low tumor metastatic potential. J Nat Cancer Inst 80(3):200–204
Leone A, Flatow U, King CR et al (1991) Reduced tumor-incidence, metastatic potential, and cytokine responsiveness of Nm23-transfected melanoma-cells. Cell 65(1):25–35
Acknowledgements
This work was supported in part by grant BCTR0504465 from the Susan G. Komen for the Cure Breast Cancer Foundation, grants from the Florida Breast Cancer Coalition Research Foundation, the Elsa U. Pardee Foundation, and the Florida State University to Dr. Q.-X. Sang, and a grant BCTR0706983 from the Susan G. Komen Breast Cancer Foundation, grant 05AA from the AFIP/ARP joint research initiative project, and grant 2006CB910505 from the Ministry of Chinese Science and Technology to Dr. Y.-G. Man.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Sahab, Z.J., Man, YG., Semaan, S.M. et al. Alteration in protein expression in estrogen receptor alpha-negative human breast cancer tissues indicates a malignant and metastatic phenotype. Clin Exp Metastasis 27, 493–503 (2010). https://doi.org/10.1007/s10585-010-9338-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10585-010-9338-8